Page 164 - Cardiac Nursing
P. 164
LWBK340-c06_p132-152.qxd 09/09/2009 08:25 AM Page 140 Aptara
140 PA R T II / Physiologic and Pathologic Responses
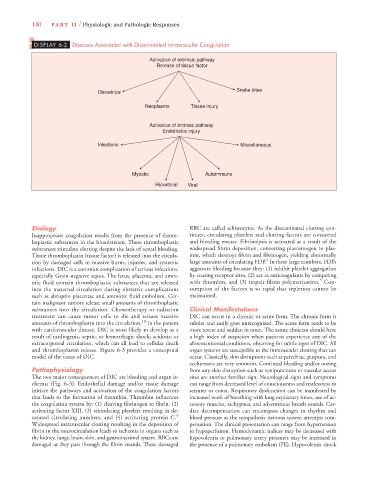
DISPLAY 6-2 Diseases Associated with Disseminated Intravascular Coagulation
Activation of extrinsic pathway
Release of tissue factor
Snake bites
Obstetrical
Neoplasms Tissue injury
Activation of intrinsic pathway
Endothelial injury
Infections Miscellaneous
Mycotic Autoimmune
Rickettsial Viral
Etiology RBC are called schistocytes. As the disseminated clotting con-
Inappropriate coagulation results from the presence of throm- tinues, circulating platelets and clotting factors are consumed
boplastic substances in the bloodstream. These thromboplastic and bleeding ensues. Fibrinolysis is activated as a result of the
substances stimulate clotting despite the lack of actual bleeding. widespread fibrin deposition, converting plasminogen to plas-
Tissue thromboplastin (tissue factor) is released into the circula- min, which destroys fibrin and fibrinogen, yielding abnormally
5
tion by damaged cells in massive burns, injuries, and systemic large amounts of circulating FDP. In these large numbers, FDPs
infections. DIC is a common complication of serious infections, aggravate bleeding because they: (1) inhibit platelet aggregation
especially Gram-negative sepsis. The fetus, placenta, and amni- by coating receptor sites, (2) act as anticoagulants by competing
5
otic fluid contain thromboplastic substances that are released with thrombin, and (3) impair fibrin polymerization. Con-
into the maternal circulation during obstetric complications sumption of the factors is so rapid that repletion cannot be
such as abruptio placentae and amniotic fluid embolism. Cer- maintained.
tain malignant tumors release small amounts of thromboplastic
substances into the circulation. Chemotherapy or radiation Clinical Manifestations
treatment can cause tumor cells to die and release massive DIC can occur in a chronic or acute form. The chronic form is
amounts of thromboplastin into the circulation. 10 In the patient subtler and easily goes unrecognized. The acute form tends to be
with cardiovascular disease, DIC is most likely to develop as a more severe and sudden in onset. The astute clinician should have
result of cardiogenic, septic, or hemorrhagic shock; acidosis; or a high index of suspicion when patients experience any of the
extracorporeal circulation, which can all lead to cellular death aforementioned conditions, observing for subtle signs of DIC. All
and thromboplastin release. Figure 6-3 provides a conceptual organ systems are susceptible to the intravascular clotting that can
model of the cause of DIC. occur. Classically, skin disruptions such as petechiae, purpura, and
ecchymosis are very common. Continual bleeding and/or oozing
Pathophysiology from any skin disruption such as venipunctures or vascular access
The two major consequences of DIC are bleeding and organ is- sites are another familiar sign. Neurological signs and symptoms
chemia (Fig. 6-3). Endothelial damage and/or tissue damage can range from decreased level of consciousness and restlessness to
initiate the pathways and activation of the coagulation factors seizures or coma. Respiratory dysfunction can be manifested by
that leads to the formation of thrombin. Thrombin influences increased work of breathing with long expiratory times, use of ac-
the coagulation system by: (1) cleaving fibrinogen to fibrin, (2) cessory muscles, tachypnea, and adventitious breath sounds. Car-
activating factor XIII, (3) stimulating platelets resulting in de- diac decompensation can encompass changes in rhythm and
creased circulating numbers, and (4) activating protein C. 5 blood pressure as the sympathetic nervous system attempts com-
Widespread intravascular clotting resulting in the deposition of pensation. The clinical presentation can range from hypertension
fibrin in the microcirculation leads to ischemia in organs such as to hypoperfusion. Hemodynamic indices may be decreased with
the kidney, lungs, brain, skin, and gastrointestinal system. RBCs are hypovolemia or pulmonary artery pressures may be increased in
damaged as they pass through the fibrin strands. These damaged the presence of a pulmonary embolism (PE). Hypovolemic shock