Page 363 - Cardiac Nursing
P. 363
M
M
6 A
Pa
g
g
Pa
6 A
c.
a
1
c.
c.
2:1
2:1
p
p
p
t
ara
ara
t
A
e 3
e 3
g
39
A
A
39
3-3
In
33
3-3
87.
87.
In
LWB
LWBK340-c16_
LWB K34 0-c 16_ p p pp333-387.qxd 6/30/09 12:16 AM Page 339 Aptara Inc.
K34
33
16_
0-c
6
6
/09
6
/09
/30
/30
q
q
a
q
1
xd
xd
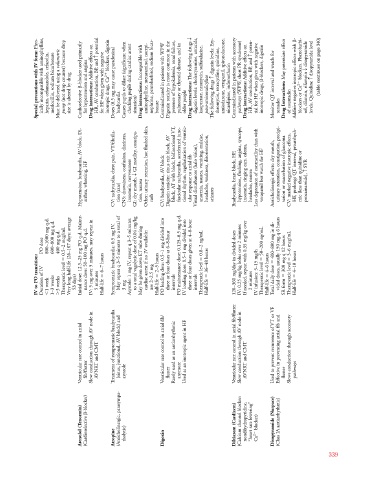
Phys- Additive effects on potential blockers, digoxin Incompatible with T digoxin levels: Ery- Additive effects on poten- May potentiate effect - blockers. Phenobarbi- disopyramide disopyramide level
Special precautions with IV form: ically incompatible with aminophylline, heparin, cefamandole, cefazolin, mezlocillin, sodium bicarbonate Must be delivered using a volumetric (not drop counter) because drop pump size is altered by drug Cardioselective -blocker used primarily for hypertension and angina Drug interactions: HR, AV conduction, BP , and c for HF when given with negative inotropic drugs, Ca 2
Doses (0.5 mg may cause paradoxical bradycardia Causes pupils to dilate (significant when checking pupils
Hypotension, bradycardia, AV block. Di- arrhea, wheezing, HF CV: tachycardia, chest pain, VT/fibrilla- tion (rare) CNS: drowsiness, confusion, dizziness, insomnia, nervousness GI motility, constipa- GI: dry mouth, T tion, nausea Other: urinary retention, hot flushed skin, rash CV: bradycardia, AV block Digoxin toxicity: sinus exit block, AV block, AT with block, bidirectional VT, fascicular tachycardia, accelerated junc- tional rhythm, regularization of ventric- ular response to atrial fib Visua
800–1600 mg q.d. 600–800 mg q.d.
PO dose 400 mg q.d. Very long half-life (26–107 days; average Initial dose: 12.5–25 mg PO q.d. Mainte- nance dose: 50–100 mg PO q.d. IV: 5 mg over 5 minutes, may repeat in Symptomatic bradycardia: 0.5 mg IV. May repeat q 3–5 minutes to a total of Asystole: 1 mg IV, repeat q 3–5 minutes to a total vagolytic dose of 0.04 mg/kg cardiac arrest if no IV available: PO loading dose: 0.5–1 mg divided into three or four doses at 6–8-hour PO maintenance dose: 0.125–0.5 mg q.d. IV loading dose: 0.5–1 mg divided into th
IV to PO transition: Duration of IV 1 week 1–3 weeks 3 weeks Therapeutic level 0.5–2 mcg/mL 53 days) 5 minutes 6–7 hours Half-life 3 mg May be given down ET tube during use 2–2.5 mg 2–5 hours Half-life intervals intervals Therapeutic level 0.8–2 ng/mL 36–48 hours Half-life 120–360 mg/day in divided doses 2 minutes IV infusion: 5–15 mg/h Therapeutic level 50–200 ng/mL 4–6 hours Half-life Total daily dose SR form Therapeutic level 3–6 mcg/mL 4–10 hours Half-life
Ventricular rate control in atrial fib/flutter Slow conduction through AV node in AVNRT and CMT Treatment of symptomatic bradycardia (sinus, junctional, AV block) and asystole Ventricular rate control in atrial fib/ flutter Rarely used as an antiarrhythmic anymore Used as an inotropic agent in HF Ventricular rate control in atrial fib/flutter Slow conduction through AV node in AVNRT and CMT Used to prevent recurrence of VT or VF Effective in preventing atrial fib and flutter Slows conduction throu
-blocker)
Atenolol (Tenormin) (Cardioselective Atropine (Anticholinergic, parasympa- tholytic) Digoxin Diltiazem (Cardizem) (Calcium channel blocker: nondihydropyridine, “heart rate lowering” blocker) Ca 2
Disopyramide (Norpace) (Class IA antiarrhythmic)
339