Page 711 - Cardiac Nursing
P. 711
51
09
P
P
M
/1/
5-7
p65
04.
7
qxd
g
K34
0-c
28_
L L LWB K34 0-c 28_ p65 5-7 04. qxd 7 /1/ 09 5: 51 P M P a a g e e 687 Ap tar a a
LWB
LWBK340-c28_p655-704.qxd 7/1/09 5:5:51 PM Page 687 Aptara
tar
Ap
687
C HAPTER 2 8 / Pacemakers and Implantable Defibrillators 687
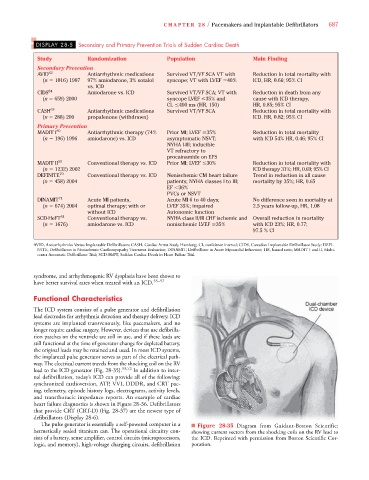
DISPLAY 28-5 Secondary and Primary Prevention Trials of Sudden Cardiac Death
Study Randomization Population Main Finding
Secondary Prevention
AVID 62 Antiarrhythmic medications Survived VT/VF SCA VT with Reduction in total mortality with
(n 1016) 1997 97% amiodarone, 3% sotalol syncope; VT with LVEF 40% ICD, HR, 0.66; 95% CI
vs. ICD
CIDS 64 Amiodarone vs. ICD Survived VT/VF SCA; VT with Reduction in death from any
(n 659) 2000 syncope LVEF 35% and cause with ICD therapy,
CL 400 ms (HR, 150) HR, 0.85; 95% CI
CASH 63 Antiarrhythmic medications Survived VT/VF SCA Reduction in total mortality with
(n 288) 200 propafenone (withdrawn) ICD. HR, 0.82; 95% CI
Primary Prevention
MADIT I 69 Antiarrhythmic therapy (74% Prior MI; LVEF 35% Reduction in total mortality
(n 196) 1996 amiodarone) vs. ICD asymptomatic NSVT; with ICD 54% HR, 0.46; 95% CI
NYHA I-III; inducible
VT refractory to
procainamide on EPS
MADIT II 50 Conventional therapy vs. ICD Prior MI; LVEF 30% Reduction in total mortality with
(n 1232) 2002 ICD therapy 31%; HR, 0.69; 95% CI
DEFINITE 70 Conventional therapy vs. ICD Nonischemic CM heart failure Trend in reduction in all cause
(n 458) 2004 patients; NYHA classes I to III; mortality by 35%; HR, 0.65
EF 36%
PVCs or NSVT
DINAMIT 71 Acute MI patients, Acute MI 6 to 40 days; No difference seen in mortality at
(n 674) 2004 optimal therapy; with or LVEF 35%; impaired 2.5 years follow-up, HR, 1.08
without ICD Autonomic function
SCD-HeFT 51 Conventional therapy vs. NYHA class II/III CHF ischemic and Overall reduction in mortality
(n 1676) amiodarone vs. ICD nonischemic LVEF 35% with ICD 23%; HR, 0.77;
97.5 % CI
AVID, Antiarrhythmics Versus Implantable Defibrillators; CASH, Cardiac Arrest Study Hamburg; CI, confidence interval; CIDS, Canadian Implantable Defibrillator Study; DEFI-
NITE, Defibrillators in Nonischemic Cardiomyopathy Treatment Evaluation; DINAMIT, Defibrillator in Acute Myocardial Infarction; HR, hazard ratio; MADIT I and II, Multi-
center Automatic Defibrillator Trial; SCD-HeFT, Sudden Cardiac Death in Heart Failure Trial.
syndrome, and arrhythmogenic RV dysplasia have been shown to
have better survival rates when treated with an ICD. 55–57
Functional Characteristics
The ICD system consists of a pulse generator and defibrillation
lead electrodes for arrhythmia detection and therapy delivery. ICD
systems are implanted transvenously, like pacemakers, and no
longer require cardiac surgery. However, devices that use defibrilla-
tion patches on the ventricle are still in use, and if these leads are
still functional at the time of generator change for depleted battery,
the original leads may be retained and used. In most ICD systems,
the implanted pulse generator serves as part of the electrical path-
way. The electrical current travels from the shocking coil on the RV
lead to the ICD generator (Fig. 28-35). 55,72 In addition to inter-
nal defibrillation, today’s ICD can provide all of the following:
synchronized cardioversion, ATP, VVI, DDDR, and CRT pac-
ing, telemetry, episode history logs, electrograms, activity levels,
and transthoracic impedance reports. An example of cardiac
heart failure diagnostics is shown in Figure 28-36. Defibrillators
that provide CRT (CRT-D) (Fig. 28-37) are the newest type of
defibrillators (Display 28-6).
The pulse generator is essentially a self-powered computer in a ■ Figure 28-35 Diagram from Guidant-Boston Scientific;
hermetically sealed titanium can. The operational circuitry con- showing current vectors from the shocking coils on the RV lead to
sists of a battery, sense amplifier, control circuits (microprocessors, the ICD. Reprinted with permission from Boston Scientific Cor-
logic, and memory), high-voltage charging circuits, defibrillation poration.