Page 304 - ACCCN's Critical Care Nursing
P. 304
Cardiac Rhythm Assessment and Management 281
Bi-V RV only
RV Bi-V
Bi-V LV only
LV Bi-V
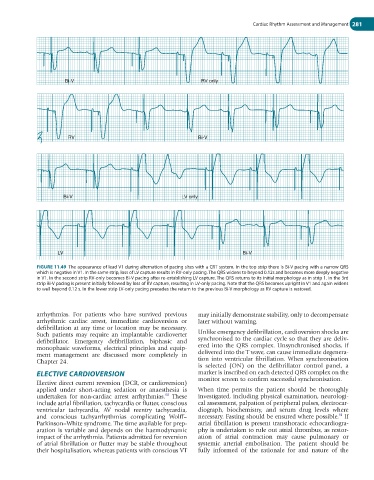
FIGURE 11.49 The appearance of lead V1 during alternation of pacing sites with a CRT system. In the top strip there is Bi-V pacing with a narrow QRS
which is negative in V1. In the same strip, loss of LV capture results in RV-only pacing. The QRS widens to beyond 0.12s and becomes more deeply negative
in V1. In the second strip RV-only becomes Bi-V pacing after re-establishing LV capture. The QRS returns to its initial morphology as in strip 1. In the 3rd
strip Bi-V pacing is present initially followed by loss of RV capture, resulting in LV-only pacing. Note that the QRS becomes upright in V1 and again widens
to well beyond 0.12 s. In the lower strip LV-only pacing precedes the return to the previous Bi-V morphology as RV capture is restored.
arrhythmias. For patients who have survived previous may initially demonstrate stability, only to decompensate
arrhythmic cardiac arrest, immediate cardioversion or later without warning.
defibrillation at any time or location may be necessary.
Such patients may require an implantable cardioverter Unlike emergency defibrillation, cardioversion shocks are
defibrillator. Emergency defibrillation, biphasic and synchronised to the cardiac cycle so that they are deliv-
monophasic waveforms, electrical principles and equip- ered into the QRS complex. Unsynchronised shocks, if
ment management are discussed more completely in delivered into the T wave, can cause immediate degenera-
Chapter 24. tion into ventricular fibrillation. When synchronisation
is selected (ON) on the defibrillator control panel, a
ELECTIVE CARDIOVERSION marker is inscribed on each detected QRS complex on the
Elective direct current reversion (DCR, or cardioversion) monitor screen to confirm successful synchronisation.
applied under short-acting sedation or anaesthesia is When time permits the patient should be thoroughly
90
undertaken for non-cardiac arrest arrhythmias. These investigated, including physical examination, neurologi-
include atrial fibrillation, tachycardia or flutter, conscious cal assessment, palpation of peripheral pulses, electrocar-
ventricular tachycardia, AV nodal reentry tachycardia, diograph, biochemistry, and serum drug levels where
91
and conscious tachyarrhythmias complicating Wolff– necessary. Fasting should be ensured where possible. If
Parkinson–White syndrome. The time available for prep- atrial fibrillation is present transthoracic echocardiogra-
aration is variable and depends on the haemodynamic phy is undertaken to rule out atrial thrombus, as restor-
impact of the arrhythmia. Patients admitted for reversion ation of atrial contraction may cause pulmonary or
of atrial fibrillation or flutter may be stable throughout systemic arterial embolisation. The patient should be
their hospitalisation, whereas patients with conscious VT fully informed of the rationale for and nature of the