Page 300 - ACCCN's Critical Care Nursing
P. 300
Cardiac Rhythm Assessment and Management 277
68 60
85/50
70
125/65
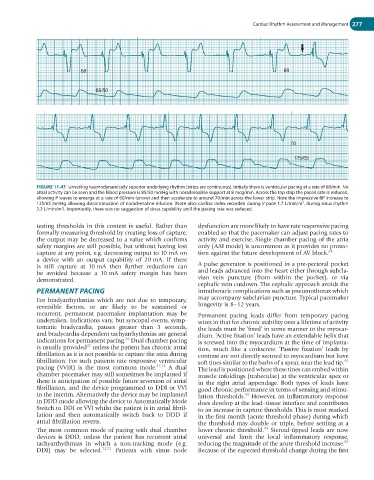
FIGURE 11.47 Unveiling haemodynamically superior underlying rhythm (strips are continuous). Initially there is ventricular pacing at a rate of 68/min. No
atrial activity can be seen and the blood pressure is 85/50 mmHg with noradrenaline support at 8 mcg/min. Across the top strip the paced rate is reduced,
allowing P waves to emerge at a rate of 60/min (arrow) and then accelerate to around 70/min across the lower strip. Note the impressive BP increase to
2
125/65 mmHg allowing discontinuation of noradrenaline infusion. (Note also: cardiac index recorded during V pace 1.7 L/min/m , during sinus rhythm
2
2.3 L/min/m ). Importantly, there was no suggestion of sinus capability until the pacing rate was reduced.
testing thresholds in this context is useful. Rather than dysfunction are more likely to have rate responsive pacing
formally measuring threshold by creating loss of capture, enabled so that the pacemaker can adjust pacing rates to
the output may be decreased to a value which confirms activity and exercise. Single chamber pacing of the atria
safety margins are still possible, but without having lost only (AAI mode) is uncommon as it provides no protec-
capture at any point, e.g. decreasing output to 10 mA on tion against the future development of AV block. 63
a device with an output capability of 20 mA. If there
is still capture at 10 mA then further reductions can A pulse generator is positioned in a pre-pectoral pocket
be avoided because a 10 mA safety margin has been and leads advanced into the heart either through subcla-
demonstrated. vian vein puncture (from within the pocket), or via
cephalic vein cutdown. The cephalic approach avoids the
PERMANENT PACING intrathoracic complications such as pneumothorax which
For bradyarrhythmias which are not due to temporary, may accompany subclavian puncture. Typical pacemaker
reversible factors, or are likely to be sustained or longevity is 8–12 years.
recurrent, permanent pacemaker implantation may be Permanent pacing leads differ from temporary pacing
undertaken. Indications vary, but syncopal events, symp- wires in that for chronic stability over a lifetime of activity
tomatic bradycardia, pauses greater than 3 seconds, the leads must be ‘fixed’ in some manner to the myocar-
and bradycardia-dependent tachyarrhythmias are general dium. ‘Active fixation’ leads have an extendable helix that
63
indications for permanent pacing. Dual chamber pacing is screwed into the myocardium at the time of implanta-
27
is usually provided unless the patient has chronic atrial tion, much like a corkscrew. ‘Passive fixation’ leads by
fibrillation as it is not possible to capture the atria during contrast are not directly secured to myocardium but have
fibrillation. For such patients rate responsive ventricular soft tines similar to the barbs of a spear, near the lead tip.
55
pacing (VVIR) is the most common mode. 27,72 A dual The lead is positioned where these tines can embed within
chamber pacemaker may still sometimes be implanted if muscle infoldings (trabeculae) at the ventricular apex or
there is anticipation of possible future reversion of atrial in the right atrial appendage. Both types of leads have
fibrillation, and the device programmed to DDI or VVI good chronic performance in terms of sensing and stimu-
in the interim. Alternatively the device may be implanted lation thresholds. However, an inflammatory response
55
in DDD mode allowing the device to Automatically Mode does develop at the lead–tissue interface and contributes
Switch to DDI or VVI whilst the patient is in atrial fibril- to an increase in capture thresholds. This is most marked
lation and then automatically switch back to DDD if in the first month (acute threshold phase) during which
atrial fibrillation reverts. the threshold may double or triple, before settling at a
55
The most common mode of pacing with dual chamber lower chronic threshold. Steroid-tipped leads are now
devices is DDD, unless the patient has recurrent atrial universal and limit the local inflammatory response,
55
tachyarrhythmias in which a non-tracking mode (e.g. reducing the magnitude of the acute threshold increase.
DDI) may be selected. 72,73 Patients with sinus node Because of the expected threshold change during the first