Page 1335 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 1335
Chapter 72 Mast Cells and Mastocytosis 1181
diagnose MCAS, and to document (other) primary and secondary or progressively increasing, or organomegaly and/or blood count
causes of MC expansion or MC activation. abnormalities emerge.
In adult patients with cutaneous MC lesions, the large majority
of such patients will ultimately be found to have SM according to
WHO diagnostic criteria. A BM biopsy is generally recommended in Survival and Prognostic Factors
these patients to establish a diagnosis of SM (see Fig. 72.7). In
patients with modest elevations of the serum tryptase level, mild or In a Mayo series of 342 patients with SM (46% ISM, 12% ASM,
no symptomology, nor evidence of blood count abnormalities or 40% SM-AHN, 1% MCL), life expectancy in ISM was similar to
11
other signs of organ damage, diagnostic testing may not elicit short- age- and sex-matched normal controls. In contrast, median OS (and
term changes in management even if SM is found. However, given leukemia-free survival) was inferior in patients with more advanced
the differences in OS between adult CM and SM, and the fact that forms of SM. For example, the median OS was 41 months and 24
only those with SM may develop severe bone disease (osteoporosis) months, respectively for ASM (n = 41 patients) and SM-AHN (n =
requiring therapy staging investigations should be extended in SM, 138 patients), and only 2 months for MCL (n = 4) patients. In a
BM analysis can be very helpful as an initial “forensic” assessment of multivariate analysis, independent adverse prognostic factors included
these potential disease trajectories. Children with skin lesions rarely advanced age, weight loss, anemia, thrombocytopenia, hypoalbumin-
11
have systemic disease. Therefore a BM biopsy is generally not recom- emia, and excess BM blasts. In addition to an increased percentage
mended in children unless the serum tryptase level is unusually high of MCs on marrow aspirate smears, Spanish investigators found that
Mast cell activation symptoms
or anaphylaxis, and/or increased
serum tryptase level ∗
(no MIS, B or C findings,
or abnormal blood counts) Adult-onset MIS ∗∗
Evaluation for systemic mastocytosis
• Bone marrow biopsy or biopsy of other
extracutaneous organ
• KIT D816V; if needed, additional KIT WHO criteria
gene sequencing for SM not
• Mast cell lmmunophenotyping fulfilled but
• Screen for FIP1L1-PDGFRA if MIS present
eosinophilia is present
Cutaneous
mastocytosis
<3 minor SM KIT wild-type At least 1 major +
criteria fulfilled and normal MC 1 minor or 3
(KIT D816V + and/or morphology/
CD25 + MC) immunophenotype minor criteria
In the absence of CM,
consider other causes for
mast cell activation Systemic
Primary (e.g., secondary MCAS) mastocytosis
MCAS or CM (allergies, drugs, infections) +/− primary
or MCAS
idiopathic MCAS/anaphylaxis
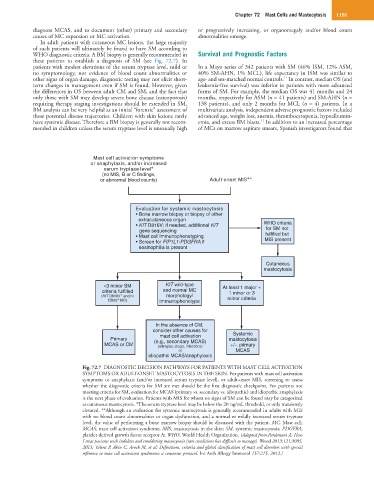
Fig. 72.7 DIAGNOSTIC DECISION PATHWAYS FOR PATIENTS WITH MAST CELL ACTIVATION
SYMPTOMS OR ADULT-ONSET MASTOCYTOSIS IN THE SKIN. For patients with mast cell activation
symptoms or anaphylaxis (and/or increased serum tryptase level), or adult-onset MIS, screening to assess
whether the diagnostic criteria for SM are met should be the first diagnostic checkpoint. For patients not
meeting criteria for SM, evaluation for MCAS (primary vs. secondary vs. idiopathic) and idiopathic anaphylaxis
is the next phase of evaluation. Patients with MIS for whom no signs of SM can be found may be categorized
as cutaneous mastocytosis. *The serum tryptase level may be below the 20 ng/mL threshold, or only transiently
elevated. **Although an evaluation for systemic mastocytosis is generally recommended in adults with MIS
with no blood count abnormalities or organ dysfunction, and a normal or mildly increased serum tryptase
level, the value of performing a bone marrow biopsy should be discussed with the patient. MC, Mast cell;
MCAS, mast cell activation syndrome; MIS, mastocytosis in the skin; SM, systemic mastocytosis; PDGFRA,
platelet-derived growth factor receptor A; WHO, World Health Organization. (Adapted from:Pardanani A: How
I treat patients with indolent and smoldering mastocytosis (rare conditions but difficult to manage). Blood 2013;121:3085,
2013; Valent P, Akin C, Arock M, et al: Definitions, criteria and global classification of mast cell disorders with special
reference to mast cell activation syndromes: a consensus protocol. Int Arch Allergy Immunol 157:215, 2012.)