Page 1846 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 1846
1642 Part X Transplantation
107
78
patients dying in the first 6 months after transplant. In another shown by Brunstein et al, 5-year NRM was 41% in DCBT patients
study, the median time to TRM was 3 months; few deaths occurred who engrafted beyond 26 days compared with 16% in patients who
after 1-year posttransplantation which resulted in 1- and 3-year OS achieved neutrophil engraftment within 26 days, which was similar
38
rates of 57% and 52% respectively. Steady immune recovery to NRM seen with other donor types. The risk of relapse at 3–5 years
observed after 6 months of transplantation likely contributes to this is about 12% to 22% after DCBT. Various studies comparing DCBT
protection against late mortality. 98 with other types of transplants showed inconsistent findings. A study
106
by Gutman et al in 31 CBT patients (87% DCBT) showed sig-
Comparison of Double-Unit Cord Blood Transplantation nificantly lower cumulative incidence of relapse at 2-years after CBT
(3.2%) compared with matched unrelated donors (MUD; 23%) and
With Adult Donor Allografts mismatched unrelated donors (MMUD; 26%). A subsequent larger
107
study by Brunstein et al similarly showed marked reduction in
A number of retrospective studies have shown comparable outcomes relapse risk at 5-year after DCBT (15%) compared with matched
after DCBT and adult donor transplantation, supporting the use of related donors (MRD; 43%), MUD (37%) and MMUD (35%), p
double-unit grafts as an alternative stem cell source (Table 107.3). < .01. However, a few recent studies involving patients with either
However, DCBT is associated with significantly prolonged engraft- single or double CBT did not find a similar advantage of relapse
ment of neutrophils and platelets, and increased NRM compared prevention after CBT. 102,108,109 However, these studies have some
with other types of allografts. 22,26,94,100,102,106–109 notable differences between CBT group and their comparative arms.
109
After myeloablative conditioning DCBT, the median time to In the study by Liu et al, there were appreciably more high-risk
neutrophil engraftment is 3 weeks and that to platelet engraftment patients in the CBT group (87%) compared with the MRD recipients
is 5 weeks approximately. 22,26,102,106–109 The risks of acute GVHD, (47%). Also, conditioning regimens differed significantly between the
especially grade III–IV (5–25%), and chronic GVHD (20–40% at 3 groups. Another study included ALL patients in complete remission
years), especially extensive, are significantly lower after DCBT com- (CR)1 and CR2, and ATG was used more commonly in the CBT
102
pared with other graft sources. 102,107,109 The risk of NRM at 2–5 year group compared with other allografts (31% versus 21%). A third
108
is typically higher after CBT (about 35–40%) than after other types study by Konuma et al included high-risk patients (65%) older
of transplants (15–35%). 107,109 One of the most important factors than 45 years of age who received CBT with methotrexate-based
contributing to high NRM is delayed neutrophil engraftment. As GVHD prophylaxis compared with MMF-based regimen used in
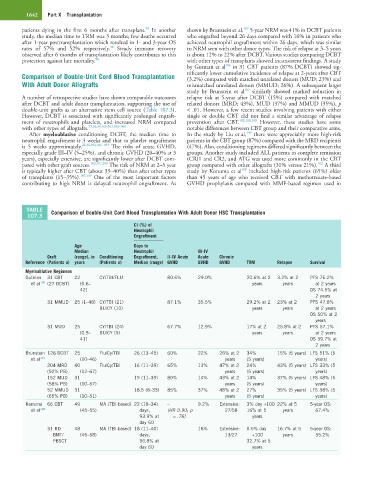
TABLE Comparison of Double-Unit Cord Blood Transplantation With Adult Donor HSC Transplantation
107.3
CI (%) of
Neutrophil
Engraftment
Age Days to
Median Neutrophil III–IV
Graft (range), in Conditioning Engraftment, II–IV Acute Acute Chronic
Reference (Patients n) years (Patients n) Median (range) GVHD GVHD GVHD TRM Relapse Survival
Myeloablative Regimens
Gutman 31 CBT 22 CY/TBI/FLU 80.6% 29.0% 20.6% at 2 3.2% at 2 PFS 76.2%
et al 106 (27 DCBT) (0.6– years years at 2 years
42) OS 74.5% at
2 years
31 MMUD 25 (1–48) CY/TBI (21) 87.1% 35.5% 29.2% at 2 23% at 2 PFS 47.8%
BU/CY (10) years years at 2 years
OS 50% at 2
years
31 MUD 25 CY/TBI (24) 67.7% 12.9% 17% at 2 25.8% at 2 PFS 57.1%
(0.9– BU/CY (5) years years at 2 years
41) OS 59.7% at
2 years
Brunstein 128 DCBT 25 Flu/Cy/TBI 26 (13–45) 60% 22% 26% at 2 34% 15% (5 years) LFS 51% (5
et al 107 (10–46) years (5 years) years)
204 MRD 40 Flu/Cy/TBI 16 (11–39) 65% 13% 47% at 2 24% 43% (5 years) LFS 33% (5
(92% PB) (12–67) years (5 years) years)
152 MUD 31 19 (11–39) 80% 14% 43% at 2 14% 37% (5 years) LFS 48% (5
(58% PB) (10–57) years (5 years) years)
52 MMUD 31 18.5 (8–33) 85% 37% 48% at 2 27% 35% (5 years) LFS 38% (5
(65% PB) (10–51) years (5 years) years)
Konuma 66 CBT 49 MA (TBI-based) 22 (18–34) – 9.2% Extensive: 3% day +100 22% at 5 5-year OS:
et al 108 (45–55) days, (HR 0.90; p 27/58 16% at 5 years 67.4%
93.9% at = .76) years
day 60
31 RD 48 MA (TBI-based) 18 (11–40) 16% Extensive: 6.5% day 16.7% at 5 5-year OS:
BMT/ (45–58) days, 13/27 +100 years 55.2%
PBSCT 96.8% at 32.7% at 5
day 60 years