Page 2381 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 2381
Chapter 144 Atherothrombosis 2123
otherwise normal, despite nearly absent LDL, suggesting that target- and Drug Administration (FDA) in 2015 as second-line therapy for
5
ing this enzyme could represent an effective strategy for cholesterol- hypercholesterolemia. In clinical trials these agents were well toler-
lowering therapeutics. Indeed, humanized monoclonal antibodies ated and lowered LDL cholesterol by approximately 60% and
inhibiting PCSK9 function were quickly developed, moved through decreased cardiovascular events by half, but it must be noted that
clinical trials (OSLER and ODYSSEY) and approved by the US Food long-term toxicity data are not yet available.
Cells in the periphery have the capacity to eliminate excess cho-
lesterol through a process known as reverse cholesterol transport (RCT).
In this pathway, summarized in Fig. 144.3, postlysosomal trafficking
of intracellular cholesterol to the plasma membrane, mediated in part
by actions of acyl-CoA cholesterol acyltransferase (ACAT) and
Niemann-Pick type C (NPC) protein, allows the cell surface adenos-
ine triphosphate (ATP)-binding cassette (ABC) proteins ABCA1 and
Lumen ABCG1 to transport excess cholesterol to apolipoprotein (apo)
A-containing lipoproteins, either nascent HDL (in the case of
ABCA1) or mature HDL (in the case of ABCG1). HDL then “deliv-
ers” the cholesterol back to the liver, where it is selectively taken up
Fatty plaque Neo-intima by hepatocytes through a protein known as scavenger receptor B1
(SRB1) and ultimately secreted into the bile and excreted in feces.
The role of HDL in RCT probably accounts for its association with
lowered risk for cardiovascular disease, but HDL particles also contain
antiinflammatory and antioxidant proteins that may also contribute
to lowering atherosclerosis risk.
Pharmacologic and lifestyle approaches to enhance RCT have
Fig. 144.1 ATHEROMATOUS PLAQUE. Cross-sectional view of a human received significant attention as potential antiatherosclerosis strate-
artery taken from an autopsy, showing accumulation of yellow-colored fatty gies. HDL levels can be raised by physical exercise, as well as by
materials in the neointima. moderate alcohol ingestion, and these are both associated with lower
Acetyl CoA + Acetoacetyl CoA
HMGCoA
↓ Low intracellular
cholesterol
STATINS
SREBP2 ↓ Mevalonic Acid
SRE SREBP2 gene
↓ Geranyl pyrophosphate
↓ Farnesyl pyrophosphate
↓ Geranylgeranyl pyrophosphate
SREBP2
SRE HMGCoA gene
↓ CHOLESTEROL ↓ Protein isoprenylation
SREBP2
SRE LDL receptor ↑ LDL Altered cell
gene
Receptors signaling
↑ LDL/VLDL
clearance
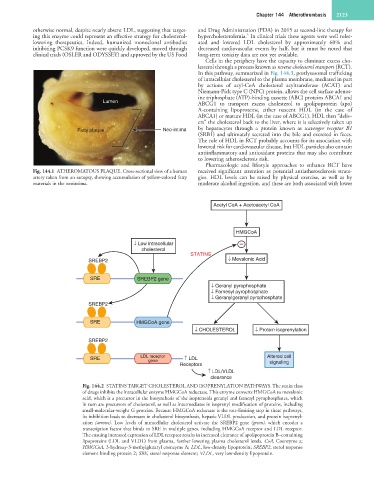
Fig. 144.2 STATINS TARGET CHOLESTEROL AND ISOPRENYLATION PATHWAYS. The statin class
of drugs inhibits the intracellular enzyme HMGCoA reductase. This enzyme converts HMGCoA to mevalonic
acid, which is a precursor in the biosynthesis of the isoprenoids geranyl and farnesyl pyrophosphates, which
in turn are precursors of cholesterol, as well as intermediates in isoprenyl modification of proteins, including
small-molecular-weight G proteins. Because HMGCoA reductase is the rate-limiting step in these pathways,
its inhibition leads to decreases in cholesterol biosynthesis, hepatic VLDL production, and protein isoprenyl-
ation (arrows). Low levels of intracellular cholesterol activate the SREBP2 gene (green), which encodes a
transcription factor that binds to SRE in multiple genes, including HMGCoA receptor and LDL receptor.
The ensuing increased expression of LDL receptor results in increased clearance of apolipoprotein B–containing
lipoproteins (LDL and VLDL) from plasma, further lowering plasma cholesterol levels. CoA, Coenzyme a;
HMGCoA, 3-hydroxy-3-methylglutaryl coenzyme A; LDL, low-density lipoprotein; SREBP2, sterol response
element binding protein 2; SRE, sterol response element; VLDL, very low-density lipoprotein.