Page 806 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 806
692 Part VI Non-Malignant Leukocytes
Sialyl Lewis Integrin receptor
carbohydrates
Selectins ICAM-1, 2
Chemotactic
receptor PECAM-1
Chemotactic
agent
Impaired integrin adhesion
Leukocyte adhesion defect I
Endothelium
Impaired E-selectin adhesion
(absent Sialyl Lewis)
Phagocytic defect Leukocyte adhesion defect II
Leukocyte adhesion defect I
Actin polymerization defect
Chediak-Higashi syndrome
Chemotactic defect
Leukocyte adhesion defect I
Chediak-Higashi syndrome
Hyper-IgE (Job) syndrome
Actin polymerization defect
Neonatal neutrophils
Localized juvenile periodontitis
Antibody
Fc receptor
Complement Bacterial killing defects
Chronic granulomatous disease
Bacteria
Chediak-Higashi syndrome
Specific granule deficiency
NADPH oxidase Neutrophil G6PD deficiency
Specific granules
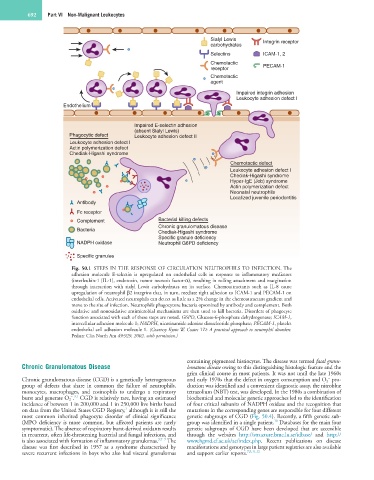
Fig. 50.1 STEPS IN THE RESPONSE OF CIRCULATION NEUTROPHILS TO INFECTION. The
adhesion molecule E-selectin is upregulated on endothelial cells in response to inflammatory mediators
(interleukin-1 [IL-1], endotoxin, tumor necrosis factor-α), resulting in rolling attachment and margination
through interaction with sialyl Lewis carbohydrates on its surface. Chemoattractants such as IL-8 cause
upregulation of neutrophil β2 integrins that, in turn, mediate tight adhesion to ICAM-1 and PECAM-1 on
endothelial cells. Activated neutrophils can detect as little as a 2% change in the chemoattractant gradient and
move to the site of infection. Neutrophils phagocytoze bacteria opsonized by antibody and complement. Both
oxidative and nonoxidative antimicrobial mechanisms are then used to kill bacteria. Disorders of phagocyte
function associated with each of these steps are noted. G6PD, Glucose-6-phosphate dehydrogenase; ICAM-1,
intercellular adhesion molecule 1; NADPH, nicotinamide adenine dinucleotide phosphate; PECAM-1, platelet
endothelial cell adhesion molecule 1. (Courtesy Kyoto W, Coates TD: A practical approach to neutrophil disorders.
Pediatr Clin North Am 49:929, 2002, with permission.)
containing pigmented histiocytes. The disease was termed fatal granu-
Chronic Granulomatous Disease lomatous disease owing to this distinguishing histologic feature and the
grim clinical course in most patients. It was not until the late 1960s
−
Chronic granulomatous disease (CGD) is a genetically heterogeneous and early 1970s that the defect in oxygen consumption and O 2 pro-
group of defects that share in common the failure of neutrophils, duction was identified and a convenient diagnostic assay, the nitroblue
monocytes, macrophages, and eosinophils to undergo a respiratory tetrazolium (NBT) test, was developed. In the 1980s a combination of
− 3,7
burst and generate O 2 . CGD is relatively rare, having an estimated biochemical and molecular genetic approaches led to the identification
incidence of between 1 in 200,000 and 1 in 250,000 live births based of four critical subunits of NADPH oxidase and the recognition that
7
on data from the United States CGD Registry, although it is still the mutations in the corresponding genes are responsible for four different
most common inherited phagocyte disorder of clinical significance genetic subgroups of CGD (Fig. 50.4). Recently, a fifth genetic sub-
10
(MPO deficiency is more common, but affected patients are rarely group was identified in a single patient. Databases for the main four
symptomatic). The absence of respiratory burst-derived oxidants results genetic subgroups of CGD have been developed that are accessible
in recurrent, often life-threatening bacterial and fungal infections, and through the websites http://structure.bmc.lu.se/idbase/ and http://
is also associated with formation of inflammatory granulomas. 3,7–9 The www.hgmd.cf.ac.uk/ac/index.php. Recent publications on disease
disease was first described in 1957 as a syndrome characterized by manifestations and genotypes in large patient registries are also available
severe recurrent infections in boys who also had visceral granulomas and support earlier reports. 7,9,11,12