Page 1165 - Clinical Immunology_ Principles and Practice ( PDFDrive )
P. 1165
83
Hematopoietic Stem Cell Transplantation for
Malignant Diseases
Pashna N. Munshi, Scott D. Rowley, Robert Korngold
Hematopoietic stem cell transplantation (HSCT) is effective treat- tumor vaccines) to induce an effective immune responsiveness
ment for most hematological malignancies, including leukemia, to the residual disease after transplantation.
lymphoma, multiple myeloma (MM), and clonal myelodysplastic
and myeloproliferative diseases (MPDs), as well as nonmalignant
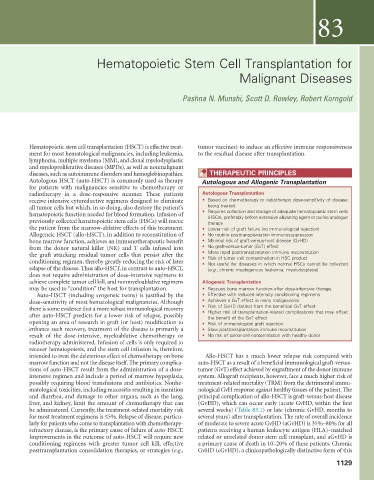
diseases, such as autoimmune disorders and hemoglobinopathies. THERAPEUTIC PRINCIPLES
Autologous HSCT (auto-HSCT) is commonly used as therapy Autologous and Allogenic Transplantation
for patients with malignancies sensitive to chemotherapy or
radiotherapy in a dose-responsive manner. These patients Autologous Transplantation
receive intensive cytoreductive regimens designed to eliminate • Based on chemotherapy or radiotherapy dose-sensitivity of disease
all tumor cells but which, in so doing, also destroy the patient’s being treated
hematopoietic function needed for blood formation. Infusion of • Requires collection and storage of adequate hematopoietic stem cells
(HSCs), preferably before extensive alkylating agent or purine analogue
previously collected hematopoietic stem cells (HSCs) will rescue therapy
the patient from the marrow-ablative effects of this treatment. • Lower risk of graft failure (no immunological rejection)
Allogeneic HSCT (allo-HSCT), in addition to reconstitution of • No routine posttransplantation immunosuppression
bone marrow function, achieves an immunotherapeutic benefit • Minimal risk of graft-versus-host disease (GvHD)
from the donor natural killer (NK) and T cells infused into • No graft-versus-tumor (GvT) effect
the graft attacking residual tumor cells that persist after the • More rapid posttransplantation immune reconstitution
• Risk of tumor cell contamination in HSC product
conditioning regimen, thereby greatly reducing the risk of later • Not useful for diseases in which normal HSCs cannot be collected
relapse of the disease. Thus allo-HSCT, in contrast to auto-HSCT, (e.g., chronic myelogenous leukemia, myelodysplasia)
does not require administration of dose-intensive regimens to
achieve complete tumor cell kill, and nonmyeloablative regimens Allogeneic Transplantation
may be used to “condition” the host for transplantation. • Rescues bone marrow function after dose-intensive therapy
Auto-HSCT (including syngeneic twins) is justified by the • Effective with reduced-intensity conditioning regimens
dose-sensitivity of most hematological malignancies. Although • Achieves a GvT effect in many malignancies
there is some evidence that a more robust immunological recovery • Risk of GvHD distinct from the beneficial GvT effect
• Higher risk of transplantation-related complications that may offset
after auto-HSCT predicts for a lower risk of relapse, possibly the benefit of the GvT effect
opening an area of research in graft (or host) modification to • Risk of immunological graft rejection
enhance such recovery, treatment of the disease is primarily a • Slow posttransplantation immune reconstitution
result of the dose-intensive, myeloablative chemotherapy or • No risk of tumor-cell contamination with healthy donor
radiotherapy administered. Infusion of cells is only required to
recover hematopoiesis, and the stem cell infusion is, therefore,
intended to treat the deleterious effect of chemotherapy on bone Allo-HSCT has a much lower relapse risk compared with
marrow function and not the disease itself. The primary complica- auto-HSCT as a result of a beneficial immunological graft-versus-
tions of auto-HSCT result from the administration of a dose- tumor (GvT) effect achieved by engraftment of the donor immune
intensive regimen and include a period of marrow hypoplasia, system. Allograft recipients, however, face a much higher risk of
possibly requiring blood transfusions and antibiotics. Nonhe- treatment-related mortality (TRM) from the detrimental immu-
matological toxicities, including mucositis resulting in inanition nological GvH response against healthy tissues of the patient. The
and diarrhea, and damage to other organs, such as the lung, principal complication of allo-HSCT is graft-versus-host disease
liver, and kidney, limit the amount of chemotherapy that can (GvHD), which can occur early (acute GvHD, within the first
be administered. Currently, the treatment-related mortality risk several weeks) (Table 83.1) or late (chronic GvHD, months to
for most treatment regimens is ≤5%. Relapse of disease, particu- several years) after transplantation. The rate of overall incidence
larly for patients who come to transplantation with chemotherapy- of moderate to severe acute GvHD (aGvHD) is 35%–80% for all
refractory disease, is the primary cause of failure of auto-HSCT. patients receiving a human leukocyte antigen (HLA)–matched
Improvements in the outcome of auto-HSCT will require new related or unrelated donor stem cell transplant, and aGvHD is
conditioning regimens with greater tumor cell kill, effective a primary cause of death in 10–20% of these patients. Chronic
posttransplantation consolidation therapies, or strategies (e.g., GvHD (cGvHD), a clinicopathologically distinctive form of this
1129