Page 419 - Clinical Immunology_ Principles and Practice ( PDFDrive )
P. 419
400 PARt tHREE Host Defenses to Infectious Agents
Gram-negative bacteria Macrophage
Release of
cytokines
Cytokine
LPS gene
expression
Nucleus
Release of LPS in vesicles or by mCD14
the action of bacteriolytic agents Mobilization of
transcription factors
LPS oligosaccharide
mCD14 Signal
MD-2 transduction
Lipid A
LBP
sCD14 TLR-4
LBP sCD14
LPS Lipopolysaccharide mCD14 Membrane-bound CD14
LBP LPS-binding protein TLR-4 Toll-like receptor 4
sCD14 Soluble CD14
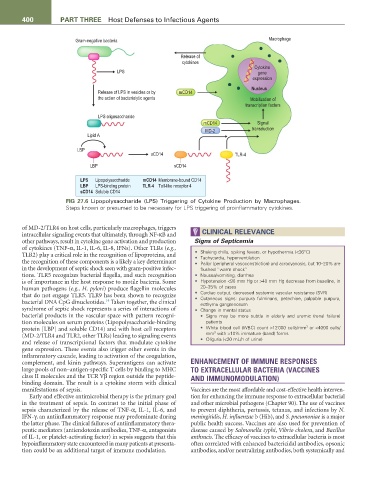
FIG 27.6 Lipopolysaccharide (LPS) Triggering of Cytokine Production by Macrophages.
Steps known or presumed to be necessary for LPS triggering of proinflammatory cytokines.
of MD-2/TLR4 on host cells, particularly macrophages, triggers
intracellular signaling events that ultimately, through NF-κB and CLINICAL RELEVANCE
other pathways, result in cytokine gene activation and production Signs of Septicemia
of cytokines (TNF-α, IL-1, IL-6, IL-8, IFNs). Other TLRs (e.g.,
TLR2) play a critical role in the recognition of lipoproteins, and • Shaking chills, spiking fevers, or hypothermia (<36°C)
• Tachycardia, hyperventilation
the recognition of these components is a likely a key determinant • Pallor (peripheral vasoconstriction) and acrocyanosis, but 10–20% are
in the development of septic shock seen with gram-positive infec- flushed “warm shock”
tions. TLR5 recognizes bacterial flagella, and such recognition • Nausea/vomiting, diarrhea
is of importance in the host response to motile bacteria. Some • Hypotension <90 mm Hg or >40 mm Hg decrease from baseline, in
human pathogens (e.g., H. pylori) produce flagellin molecules 20–35% of cases
that do not engage TLR5. TLR9 has been shown to recognize • Cardiac output, decreased systemic vascular resistance (SVR)
• Cutaneous signs: purpura fulminans, petechiae, palpable purpura,
14
bacterial DNA CpG dinucleotides. Taken together, the clinical ecthyma gangrenosum
syndrome of septic shock represents a series of interactions of • Change in mental status
bacterial products in the vascular space with pattern recogni- • Signs may be more subtle in elderly and uremic (renal failure)
tion molecules on serum proteins (Lipopolysaccharide-binding patients
3
protein [LBP] and soluble CD14) and with host cell receptors • White blood cell (WBC) count >12 000 cells/mm or <4000 cells/
3
(MD-2/TLR4 and TLR2, other TLRs) leading to signaling events mm with >10% immature (band) forms
and release of transcriptional factors that modulate cytokine • Oliguria (<20 mL/h of urine)
gene expression. These events also trigger other events in the
inflammatory cascade, leading to activation of the coagulation,
complement, and kinin pathways. Superantigens can activate ENHANCEMENT OF IMMUNE RESPONSES
large pools of non–antigen-specific T cells by binding to MHC TO EXTRACELLULAR BACTERIA (VACCINES
class II molecules and the TCR Vβ region outside the peptide- AND IMMUNOMODULATION)
binding domain. The result is a cytokine storm with clinical
manifestations of sepsis. Vaccines are the most affordable and cost-effective health interven-
Early and effective antimicrobial therapy is the primary goal tion for enhancing the immune response to extracellular bacterial
in the treatment of sepsis. In contrast to the initial phase of and other microbial pathogens (Chapter 90). The use of vaccines
sepsis characterized by the release of TNF-α, IL-1, IL-6, and to prevent diphtheria, pertussis, tetanus, and infections by N.
IFN-γ, an antiinflammatory response may predominate during meningitidis, H. influenzae b (Hib), and S. pneumoniae is a major
the latter phase. The clinical failures of antiinflammatory thera- public health success. Vaccines are also used for prevention of
peutic mediators (antiendotoxin antibodies, TNF-α, antagonists disease caused by Salmonella typhi, Vibrio cholera, and Bacillus
of IL-1, or platelet-activating factor) in sepsis suggests that this anthracis. The efficacy of vaccines to extracellular bacteria is most
hypoinflammatory state encountered in many patients at presenta- often correlated with enhanced bactericidal antibodies, opsonic
tion could be an additional target of immune modulation. antibodies, and/or neutralizing antibodies, both systemically and