Page 451 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 451
CHAPTER 39: Pulmonary Embolic Disorders: Thrombus, Air, and Fat 321
30 TABLE 39-1 Symptoms and Signs of Pulmonary Embolism 19,28
Symptom Incidence (%) Sign Incidence (%)
25 distention Dyspnea 80 Tachypnea 90
Left ventricular diastolic pressure 15 Apprehension 60 Tachycardia 2 50 8
Acute RV
Fever
70
Pleuritic pain
50
20
50
Cough
Increased 2nd heart sound (P )
50
Signs of DVT
35
33
Symptoms of DVT
Hemoptysis
25
Shock
10
https://kat.cr/user/tahir99/
Palpitations
10
5
Normal Central chest pain 10 5
Syncope
0
60 70 80 90 100 110 120 130 140
Left ventricular volume
to a diagnosis of PE. Rare patients with PE have disseminated intravas-
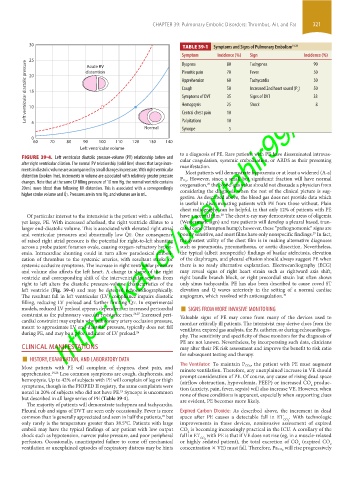
FIGURE 39-4. Left ventricular diastolic pressure-volume (PV) relationship before and cular coagulation, systemic embolization, or ARDS as their presenting
after right ventricular dilation. The normal PV relationship (solid line) shows that large incre- manifestation.
ments in diastolic volume are accompanied by small changes in pressure. With right ventricular Most patients will demonstrate hypoxemia or at least a widened (A-a)
distention (broken line), increments in volume are associated with relatively greater pressure . However, since a small but significant fraction will have normal
changes. Note that at the same LV filling pressure of 10 mm Hg, the normal ventricle contains P O 2 20
oxygenation, the blood-gas value should not dissuade a physician from
20 mL more blood than following RV distention. This is associated with a correspondingly considering the diagnosis when the rest of the clinical picture is sug-
˙
higher stroke volume and Qt. Pressures are in mm Hg, and volumes are in mL.
gestive. As described above, the blood gas does not provide data which
is useful in discriminating patients with PE from those without. Plain
chest radiography can be helpful, in that only 12% of patients with PE
Of particular interest to the intensivist is the patient with a sublethal, have a normal film. The chest x-ray may demonstrate areas of oligemia
29
yet large, PE. With increased afterload, the right ventricle dilates to a (Westermark sign) and rare patients will develop a pleural based, trun-
larger end-diastolic volume. This is associated with elevated right atrial cated cone (Hampton hump); however, these “pathognomonic” signs are
and ventricular pressures and abnormally low Q ˙ t. One consequence poorly sensitive, and most films have only nonspecific findings. In fact,
29
of raised right atrial pressure is the potential for right-to-left shunting the greatest utility of the chest film is in making alternative diagnoses
across a probe patent foramen ovale, causing oxygen-refractory hypox- such as pneumonia, pneumothorax, or aortic dissection. Nevertheless,
emia. Intracardiac shunting could in turn allow paradoxical emboli- the typical (albeit nonspecific) findings of basilar atelectasis, elevation
zation of thrombus to the systemic arteries, with resultant stroke or of the diaphragm, and pleural effusion should always suggest PE when
systemic occlusive symptoms. The increase in right ventricular pressure there is no ready alternative explanation. Electrocardiography (ECG)
and volume also affects the left heart. A change in shape of the right may reveal signs of right heart strain such as rightward axis shift,
ventricle and corresponding shift of the interventricular septum from right bundle branch block, or right precordial strain but often shows
right to left alters the diastolic pressure-volume characteristics of the only sinus tachycardia. PE has also been described to cause coved ST
left ventricle (Fig. 39-4) and may be detected echocardiographically. elevation and Q waves anteriorly in the setting of a normal cardiac
The resultant fall in left ventricular (LV) compliance impairs diastolic angiogram, which resolved with anticoagulation. 30
filling, reducing LV preload and further limiting Q ˙ t. In experimental
models, reduced LV preload appears dependent on increased pericardial ■ SIGNS FROM MORE INVASIVE MONITORING
constraint as the pulmonary vascular resistance rises. 26,27 Increased peri- Valuable signs of PE may come from many of the devices used to
cardial constraint may explain why pulmonary artery occlusion pressure, monitor critically ill patients. The intensivist may derive clues from the
meant to approximate LV end-diastolic pressure, typically does not fall ventilator, expired gas analysis, the Pa catheter, or during echocardiogra-
during PE, and may be a poor indicator of LV preload. 26 phy. The sensitivity and specificity of these monitors for the diagnosis of
PE are not known. Nevertheless, by incorporating such data, clinicians
CLINICAL MANIFESTATIONS may alter their PE risk assessment and improve the benefit to risk ratio
■ HISTORY, EXAMINATION, AND LABORATORY DATA for subsequent testing and therapy.
Most patients with PE will complain of dyspnea, chest pain, and The Ventilator: To maintain P CO 2 , the patient with PE must augment
minute ventilation. Therefore, any unexplained increase in VE should
apprehension. 19,28 Less common symptoms are cough, diaphoresis, and prompt consideration of PE. Of course, any cause of rising dead space
hemoptysis. Up to 42% of subjects with PE will complain of leg or thigh (airflow obstruction, hypovolemia, PEEP) or increased CO produc-
symptoms, though in the PIOPED II registry, the same complaints were tion (anxiety, pain, fever, sepsis) will also increase VE. However, when
2
noted in 20% of subjects who did not have PE. Syncope is uncommon none of these conditions is apparent, especially when supporting clues
19
but described in all large series of PE (Table 39-1). are evident, PE becomes more likely.
The majority of patients will demonstrate tachypnea and tachycardia.
Pleural rub and signs of DVT are seen only occasionally. Fever is more Expired Carbon Dioxide: As described above, the increment in dead
common than is generally appreciated and seen in half the patients, but space after PE causes a detectable fall in ET . With technologic
28
CO 2
only rarely is the temperature greater than 38.5°C. Patients with large improvements in these devices, noninvasive assessment of expired
emboli may have the typical findings of any patient with low output CO is becoming increasingly practical in the ICU. A corollary of the
2
shock such as hypotension, narrow pulse pressure, and poor peripheral fall in ET with PE is that if VE does not rise (eg, in a muscle-relaxed
CO 2
perfusion. Occasionally, unanticipated failure to come off mechanical or highly sedated patient), the total excretion of CO (expired CO
2
2
ventilation or unexplained episodes of respiratory distress may be hints concentration × VE) must fall. Therefore, Pa CO 2 will rise progressively
section03.indd 321 1/23/2015 2:07:32 PM