Page 453 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 453
CHAPTER 39: Pulmonary Embolic Disorders: Thrombus, Air, and Fat 323
Treat; PPV only 60%
+
Stop
NPV 96%
–
Helical CT Treat
– NO –
Low + Abnormal YES +
D-Dimer LE Duplex
leg exam
https://kat.cr/user/tahir99/
Pretest Intermediate – STOP
probability Helical CT NPV 89%
+
Treat; PPV > 92% STOP
+ Treat
ECHO RV
+ Strain*
–
NPV 60% + +
High † – – –
Helical CT LE Duplex PA Gram
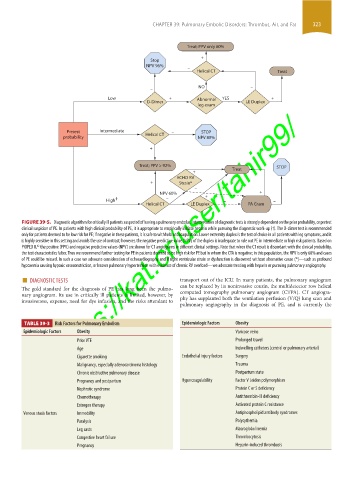
FIGURE 39-5. Diagnostic algorithm for critically ill patients suspected of having a pulmonary embolus. Interpretation of diagnostic tests is strongly dependent on the prior probability, or pretest
clinical suspicion of PE. In patients with high clinical probability of PE, it is appropriate to empirically initiate heparin while pursuing the diagnostic work-up (†). The D-dimer test is recommended
only for patients deemed to be low risk for PE; if negative in these patients, it is safe to withhold anticoagulation. Lower extremity duplex is the test of choice in all patients with leg symptoms, and it
is highly sensitive in this setting and avoids the use of contrast; however, the negative predictive value (NPV) of the duplex is inadequate to rule out PE in intermediate or high risk patients. Based on
42
PIOPED II, the positive (PPV) and negative predictive values (NPV) are shown for CT angiograms in different clinical settings. Note that when the CT result is discordant with the clinical probability,
the test characteristics falter. Thus we recommend further testing for PE in patients deemed to be high risk for PE but in whom the CTA is negative; in this population, the NPV is only 60% and cases
of PE could be missed. In such a case we advocate consideration of echocardiography and if right ventricular strain or dysfunction is discovered without alternative cause (*)—such as profound
hypoxemia causing hypoxic vasoconstriction, or known pulmonary hypertension with evidence of chronic RV overload—we advocate treating with heparin or pursuing pulmonary angiography.
■ DIAGNOSTIC TESTS transport out of the ICU. In many patients, the pulmonary angiogram
The gold standard for the diagnosis of PE has long been the pulmo- can be replaced by its noninvasive cousin, the multidetector row helical
nary angiogram. Its use in critically ill patients is limited, however, by computed tomography pulmonary angiogram (CTPA). CT angiogra-
phy has supplanted both the ventilation perfusion (V/Q) lung scan and
invasiveness, expense, need for dye infusion, and the risks attendant to
pulmonary angiography in the diagnosis of PE, and is currently the
TABLE 39-3 Risk Factors for Pulmonary Embolism Epidemiologic Factors Obesity
Epidemiologic Factors Obesity Varicose veins
Prior VTE Prolonged travel
Age Indwelling catheters (central or pulmonary arterial)
Cigarette smoking Endothelial injury factors Surgery
Malignancy, especially adenocarcinoma histology Trauma
Chronic obstructive pulmonary disease Postpartum state
Pregnancy and postpartum Hypercoagulability Factor V Leiden polymorphism
Nephrotic syndrome Protein C or S deficiency
Chemotherapy Antithrombin-III deficiency
Estrogen therapy Activated protein C resistance
Venous stasis factors Immobility Antiphospholipid antibody syndromes
Paralysis Polycythemia
Leg casts Macroglobulinemia
Congestive heart failure Thrombocytosis
Pregnancy Heparin-induced thrombosis
section03.indd 323 1/23/2015 2:07:34 PM