Page 659 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 659
478 PART 4: Pulmonary Disorders
180 patients. Of the 90 conventional treatment patients, 41 survived.
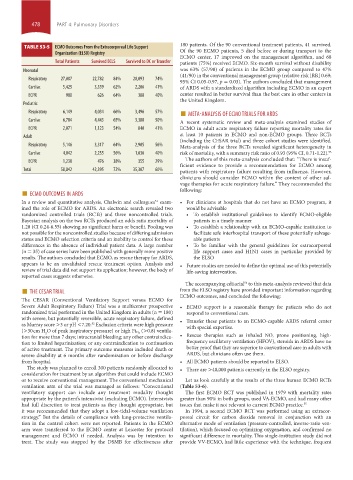
TABLE 53-5 ECMO Outcomes From the Extracorporeal Life Support
Organization (ELSO) Registry Of the 90 ECMO patients, 5 died before or during transport to the
ECMO center, 17 improved on the management algorithm, and 68
Total Patients Survived ECLS Survived to DC or Transfer patients (75%) received ECMO. Six-month survival without disability
Neonatal was 63% (57/90) of patients in the ECMO group compared to 47%
(41/90) in the conventional management group (relative risk [RR] 0.69;
Respiratory 27,007 22,782 84% 20,093 74%
95% CI 0.05-0.97, p = 0.03). The authors concluded that management
Cardiac 5,425 3,339 62% 2,206 41% of ARDS with a standardized algorithm including ECMO in an expert
ECPR 980 626 64% 388 40% center resulted in better survival than the best care in other centers in
the United Kingdom.
Pediatric
Respiratory 6,149 4,034 66% 3,496 57% ■ META-ANALYSIS OF ECMO TRIALS FOR ARDS
Cardiac 6,784 4,443 65% 3,388 50% A recent systematic review and meta-analysis examined studies of
ECPR 2,071 1,123 54% 840 41% ECMO in adult acute respiratory failure reporting mortality rates for
Adult at least 10 patients in ECMO and non-ECMO groups. Three RCTs
(including the CESAR trial) and three cohort studies were identified.
Respiratory 5,146 3,317 64% 2,905 56% Meta-analysis of the three RCTs revealed significant heterogeneity in
Cardiac 4,042 2,255 56% 1,636 40% risk of mortality, with a summary risk ratio of 0.93 (95% CI, 0.71-1.22). 53
The authors of this meta-analysis concluded that: “There is insuf-
ECPR 1,238 476 38% 355 29%
ficient evidence to provide a recommendation for ECMO among
Total 58,842 42,395 72% 35,307 60% patients with respiratory failure resulting from influenza. However,
clinicians should consider ECMO within the context of other sal-
vage therapies for acute respiratory failure.” They recommended the
■ ECMO OUTCOMES IN ARDS following:
In a review and quantitative analysis, Chalwin and colleagues exam- • For clinicians at hospitals that do not have an ECMO program, it
51
ined the role of ECMO for ARDS. An electronic search revealed two would be advisable
randomized controlled trials (RCTs) and three noncontrolled trials. • To establish institutional guidelines to identify ECMO-eligible
Bayesian analysis on the two RCTs produced an odds ratio mortality of patients in a timely manner
1.28 (CI 0.24-6.55) showing no significant harm or benefit. Pooling was • To establish a relationship with an ECMO-capable institution to
not possible for the noncontrolled studies because of differing admission facilitate safe interhospital transport of these potentially salvage-
status and ECMO selection criteria and an inability to control for these able patients
differences in the absence of individual patient data. A large number • To be familiar with the general guidelines for extracorporeal
(n = 35) of case series have been published with generally more positive life support cases and H1N1 cases in particular provided by
results. The authors concluded that ECMO, as rescue therapy for ARDS, the ELSO
appears to be an unvalidated rescue treatment option. Analysis and • Future studies are needed to define the optimal use of this potentially
review of trial data did not support its application; however, the body of life-saving intervention.
reported cases suggests otherwise.
■ THE CESAR TRIAL from the ELSO registry have provided important information regarding
The accompanying editorial to this meta-analysis reviewed that data
54
The CESAR (Conventional Ventilatory Support versus ECMO for ECMO outcomes, and concluded the following:
Severe Adult Respiratory Failure) Trial was a multicenter prospective • ECMO support is a reasonable therapy for patients who do not
randomized trial performed in the United Kingdom in adults (n = 180) respond to conventional care.
with severe, but potentially reversible, acute respiratory failure, defined • Transfer these patients to an ECMO-capable ARDS referral center
as Murray score >3 or pH <7.20. Exclusion criteria were high pressure with special expertise.
52
(>0.8) ventila-
2
(>30 cm H O of peak inspiratory pressure) or high Fi O 2
tion for more than 7 days; intracranial bleeding; any other contraindica- • Rescue therapies such as inhaled NO, prone positioning, high-
tion to limited heparinization; or any contraindication to continuation frequency oscillatory ventilation (HFOV), steroids in ARDS have no
of active treatment. The primary outcome measures included death or better proof that they are superior to conventional care in adults with
severe disability at 6 months after randomization or before discharge ARDS, but clinicians often use them.
from hospital. • All ECMO patients should be reported to ELSO.
The study was planned to enroll 300 patients randomly allocated to • There are >40,000 patients currently in the ELSO registry.
consideration for treatment by an algorithm that could include ECMO
or to receive conventional management. The conventional mechanical Let us look carefully at the results of the three human ECMO RCTs
ventilation arm of the trial was managed as follows: “Conventional (Table 53-6).
ventilatory support can include any treatment modality thought The first ECMO RCT was published in 1979 with mortality rates
appropriate by the patient’s intensivist (excluding ECMO). Intensivists greater than 90% in both groups, used VA-ECMO, and had many other
had full discretion to treat patients as they thought appropriate, but issues that make it not relevant to current ECMO practice. 55
it was recommended that they adopt a low-tidal-volume ventilation In 1994, a second ECMO RCT was performed using an extracor-
strategy.” But the details of compliance with lung-protective ventila- poreal circuit for carbon dioxide removal in conjunction with an
tion in the control cohort were not reported. Patients in the ECMO alternative mode of ventilation (pressure-controlled, inverse-ratio ven-
arm were transferred to the ECMO center at Leicester for protocol tilation), which focused on optimizing oxygenation, and confirmed no
management and ECMO if needed. Analysis was by intention to significant difference in mortality. This single-institution study did not
treat. The study was stopped by the DSMB for effectiveness after provide VV-ECMO, had little experience with the technique, frequent
section04.indd 478 1/23/2015 2:20:01 PM