Page 236 - The Netter Collection of Medical Illustrations - Integumentary System_ Volume 4 ( PDFDrive )
P. 236
Plate 8-13 Integumentary System
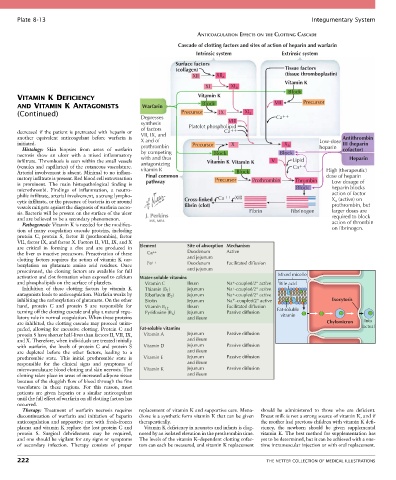
ANTICOAGULATION EFFECTS ON THE CLOTTING CASCADE
Cascade of clotting factors and sites of action of heparin and warfarin
Intrinsic system Extrinsic system
Surface factors
(collagen) Tissue factors
XII XII a (tissue thromboplastin)
Vitamin K
XI XI a
Block
VITAMIN K DEFICIENCY Vitamin K Precursor
AND VITAMIN K ANTAGONISTS Warfarin Block VII
(Continued) Precursor IX XI a
Depresses Ca
synthesis VIII
of factors Platelet phospholipid
decreased if the patient is pretreated with heparin or VII, IX, and Ca
another equivalent anticoagulant before warfarin is X and of Antithrombin
initiated. prothrombin Precursor X X a Low-dose III (heparin
Histology: Skin biopsies from areas of warfarin heparin cofactor)
necrosis show an ulcer with a mixed inflammatory by competing Block Block
with and thus
infiltrate. Thrombosis is seen within the small vessels antagonizing Vitamin K Vitamin K V Lipid Heparin
(venules and capillaries) of the cutaneous vasculature. vitamin K Ca
Arterial involvement is absent. Minimal to no inflam- Block High (therapeutic)
matory infiltrate is present. Red blood cell extravasation Final common Precursor Prothrombin Thrombin dose of heparin
is prominent. The main histopathological finding is pathway Low dosage of
microthrombi. Findings of inflammation, a neutro- Block heparin blocks
philic infiltrate, arterial involvement, a strong lympho- Ca XIII action of factor
cytic infiltrate, or the presence of bacteria in or around Cross-linked X a (active) on
vessels mitigate against the diagnosis of warfarin necro- fibrin (clot) prothrombin, but
sis. Bacteria will be present on the surface of the ulcer Fibrin Fibrinogen larger doses are
and are believed to be a secondary phenomenon. required to block
Pathogenesis: Vitamin K is needed for the modifica- action of thrombin
tion of many coagulation cascade proteins, including on fibrinogen.
protein C, protein S, factor II (prothrombin), factor
VII, factor IX, and factor X. Factors II, VII, IX, and X
are critical in forming a clot and are produced in Element Site of absorption Mechanism
the liver as inactive precursors. Preactivation of these Ca ++ Duodenum Active
clotting factors requires the action of vitamin K car- ++ and jejunum
boxylation on glutamate amino acid residues. Once Fe Duodenum Facilitated diffusion
preactivated, the clotting factors are available for full and jejunum
activation and clot formation when exposed to calcium Water-soluble vitamins Mixed micelle
and phospholipids on the surface of platelets. Vitamin C Ileum Na + -coupled/2° active Bile acid
Inhibition of these clotting factors by vitamin K Thiamin (B ) Jejunum Na -coupled/2° active
+
1
antagonists leads to anticoagulation. Warfarin works by Riboflavin (B ) Jejunum Na -coupled/2° active
+
2
inhibiting the carboxylation of glutamate. On the other Biotin Jejunum Na -coupled/2° active Exocytosis
+
hand, protein C and protein S are responsible for Vitamin B 12 Ileum Facilitated diffusion
turning off the clotting cascade and play a natural regu- Pyridoxine (B ) Jejunum Passive diffusion Fat-soluble
6
latory role in normal coagulation. When these proteins and ileum vitamin
are inhibited, the clotting cascade may proceed unim- Chylomicron Into
peded, allowing for excessive clotting. Protein C and Fat-soluble vitamins lacteal
protein S have shorter half-lives than factors II, VII, IX, Vitamin A Jejunum Passive diffusion
and X. Therefore, when individuals are treated initially and ileum
with warfarin, the levels of protein C and protein S Vitamin D Jejunum Passive diffusion
are depleted before the other factors, leading to a and ileum
prothrombic state. This initial prothrombic state is Vitamin E Jejunum Passive diffusion
responsible for the clinical signs and symptoms of and ileum
microvasculature blood clotting and skin necrosis. The Vitamin K Jejunum Passive diffusion
clotting takes place in areas of increased adipose tissue and ileum
because of the sluggish flow of blood through the fine
vasculature in these regions. For this reason, most
patients are given heparin or a similar anticoagulant
until the full effect of warfarin on all clotting factors has
occurred.
Therapy: Treatment of warfarin necrosis requires replacement of vitamin K and supportive care. Mena- should be administered to those who are deficient.
discontinuation of warfarin and initiation of heparin dione is a synthetic form vitamin K that can be given Breast milk is not a strong source of vitamin K, and if
anticoagulation and supportive care with fresh-frozen therapeutically. the mother had previous children with vitamin K defi-
plasma and vitamin K replace the lost protein C and Vitamin K deficiency in neonates and infants is diag- ciency, the newborn should be given supplemental
protein S. Surgical debridement may be required, nosed by an isolated elevation in the prothrombin time. vitamin K. The best method for supplementation has
and one should be vigilant for any signs or symptoms The levels of the vitamin K–dependent clotting cofac- yet to be determined, but it can be achieved with a one-
of secondary infection. Therapy consists of proper tors can each be measured, and vitamin K replacement time intramuscular injection or with oral replacement.
222 THE NETTER COLLECTION OF MEDICAL ILLUSTRATIONS