Page 408 - Cardiac Nursing
P. 408
1
1
1
/09
/09
/09
6 A
M
M
2:1
2:1
6 A
/30
87.
q
q
3-3
3-3
87.
6
6
/30
q
xd
xd
Pa
t
ara
ara
p
p
t
In
c.
c.
a
a
In
p
g
g
e 3
Pa
Pa
g
84
A
A
e 3
84
84
LWB
LWB K34 0-c 16_ p p pp333-387.qxd 6/30/09 12:16 AM Page 384 Aptara Inc.
33
LWBK340-c16_
16_
0-c
K34
33
384 P A R T III / Assessment of Heart Disease
V 1
V 1
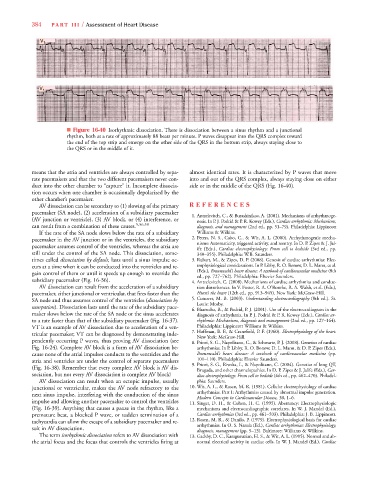
■ Figure 16-40 Isorhythmic dissociation. There is dissociation between a sinus rhythm and a junctional
rhythm, both at a rate of approximately 88 beats per minute. P waves disappear into the QRS complex toward
the end of the top strip and emerge on the other side of the QRS in the bottom strip, always staying close to
the QRS or in the middle of it.
means that the atria and ventricles are always controlled by sepa- almost identical rates. It is characterized by P waves that move
rate pacemakers and that the two different pacemakers never con- into and out of the QRS complex, always staying close on either
duct into the other chamber to “capture” it. Incomplete dissocia- side or in the middle of the QRS (Fig. 16-40).
tion occurs when one chamber is occasionally depolarized by the
other chamber’s pacemaker.
AV dissociation can be secondary to (1) slowing of the primary R EFEREN C E S
pacemaker (SA node), (2) acceleration of a subsidiary pacemaker
1. Antzelevitch, C., & Burashinikov, A. (2001). Mechanisms of arrhythmoge-
(AV junction or ventricle), (3) AV block, or (4) interference, or nesis. In P. J. Podrid & P. R. Kowey (Eds.), Cardiac arrhythmia: Mechanisms,
can result from a combination of these causes. 5,56,58 diagnosis, and management (2nd ed., pp. 51–79). Philadelphia: Lippincott
If the rate of the SA node slows below the rate of a subsidiary Williams & Wilkins.
pacemaker in the AV junction or in the ventricles, the subsidiary 2. Peters, N. S., Cabo, C., & Wit, A. L. (2000). Arrhythmogenic mecha-
nisms: Automaticity, triggered activity, and reentry. In D. P. Zipes & J. Jal-
pacemaker assumes control of the ventricles, whereas the atria are
ife (Eds.), Cardiac electrophysiology: From cell to bedside (3rd ed., pp.
still under the control of the SA node. This dissociation, some- 340–355). Philadelphia: W.B. Saunders.
t
times called dissociation by default, lasts until a sinus impulse oc- 3. Rubart, M., & Zipes, D. P. (2008). Genesis of cardiac arrhythmias: Elec-
t
curs at a time when it can be conducted into the ventricles and re- trophysiological considerations. In P. Libby, R. O. Bonow, D. L. Mann, et al.
(Eds.), Braunwald’s heart disease: A textbook of cardiovascular medicine (8th
gain control of them or until it speeds up enough to override the
ed., pp. 727–762). Philadelphia: Elsevier Saunders.
subsidiary pacemaker (Fig. 16-36). 4. Antzelevitch, C. (2008). Mechanisms of cardiac arrhythmias and conduc-
AV dissociation can result from the acceleration of a subsidiary tion disturbances. In V. Fuster, R. A. O’Rourke, R. A. Walsh, et al. (Eds.),
pacemaker, either junctional or ventricular, that fires faster than the Hurst’s the heart (12th ed., pp. 913–945). New York: McGraw-Hill.
SA node and thus assumes control of the ventricles (dissociation by 5. Conover, M. B. (2003). Understanding electrocardiography (8th ed.). St.
Louis: Mosby.
usurpation). Dissociation lasts until the rate of the subsidiary pace-
6.Bharucha, B., & Podrid, P. J. (2001). Use of the electrocardiogram in the
maker slows below the rate of the SA node or the sinus accelerates diagnosis of arrhythmia. In P. J. Podrid & P. R. Kowey (Eds.), Cardiac ar-
to a rate faster than that of the subsidiary pacemaker (Fig. 16-37). rhythmia: Mechanisms, diagnosis and management (2nd ed., pp. 127–164).
VT is an example of AV dissociation due to acceleration of a ven- Philadelphia: Lippincott Williams & Wilkins.
7.Hoffman, B. F., & Cranefield, P. F. (1960). Electrophysiology of the heart.
tricular pacemaker; VT can be diagnosed by demonstrating inde-
New York: McGraw-Hill.
pendently occurring P waves, thus proving AV dissociation (see 8. Priori, S. G., Napolitano, C., & Schwartz, P. J. (2008). Genetics of cardiac
Fig. 16-24). Complete AV block is a form of AV dissociation be- arrhythmias. In P. Libby, R. O. Bonow, D. L. Mann, & D. P. Zipes (Eds.),
cause none of the atrial impulses conducts to the ventricles and the Braunwald’s heart disease: A textbook of cardiovascular medicine (pp.
atria and ventricles are under the control of separate pacemakers 101–110). Philadelphia: Elsevier Saunders.
9. Priori, S. G., Rivolta, I., & Napolitano, C. (2004). Genetics of long QT,
(Fig. 16-38). Remember that every complete AV block is AV dis-
Brugada, and other channelopathies. In D. P. Zipes & J. Jalife (Eds.), Car-
sociation, but not every AV dissociation is complete AV block! diac electrophysiology: From cell to bedside (4th ed., pp. 462–470). Philadel-
AV dissociation can result when an ectopic impulse, usually phia: Saunders.
junctional or ventricular, makes the AV node refractory to the 10. Wit, A. L., & Rosen, M. R. (1981). Cellular electrophysiology of cardiac
arrhythmias. Part I: Arrhythmias caused by abnormal impulse generation.
next sinus impulse, interfering with the conduction of the sinus
Modern Concepts in Cardiovascular Disease, 50, 1–6.
impulse and allowing another pacemaker to control the ventricles 11. Singer, D. H., & Cohen, H. C. (1995). Aberrancy: Electrophysiologic
(Fig. 16-39). Anything that causes a pause in the rhythm, like a mechanisms and electrocardiographic correlates. In W. J. Mandel (Ed.),
premature beat, a blocked P wave, or sudden termination of a Cardiac arrhythmias (3rd ed., pp. 461–503). Philadelphia: J. B. Lippincott.
tachycardia can allow the escape of a subsidiary pacemaker and re- 12. Rosen, M. R., & Danilo, P. (1979). Electrophysiological basis for cardiac
arrhythmias. In O. S. Narula (Ed.), Cardiac arrhythmias: Electrophysiology,
sult in AV dissociation.
diagnosis, management (pp. 9–13). Baltimore: Williams & Wilkins.
The term isorhythmic dissociation refers to AV dissociation with 13. Gadsby, D. C., Karagueuzian, H. S., & Wit, A. L. (1995). Normal and ab-
the atrial focus and the focus that controls the ventricles firing at normal electrical activity in cardiac cells. In W. J. Mandel (Ed.), Cardiac