Page 540 - Cardiac Nursing
P. 540
q
Pa
q
q
3
3
xd
xd
g
g
g
e 5
e 5
36.
36.
1-5
1-5
1
1
009
009
0 A
0 A
1:0
1:0
6/2
0/0
0/0
3
Pa
M
6/2
M
M
ara
LWB
LWBK340-c22_
t
ara
ara
K34
22_
0-c
51
51
p
t
16
16
A
A
p
p
p
LWB K34 0-c 22_ p pp511-536.qxd 30/06/2009 11:00 AM Page 516 Aptara
516 PA R T I V / Pathophysiology and Management of Heart Disease
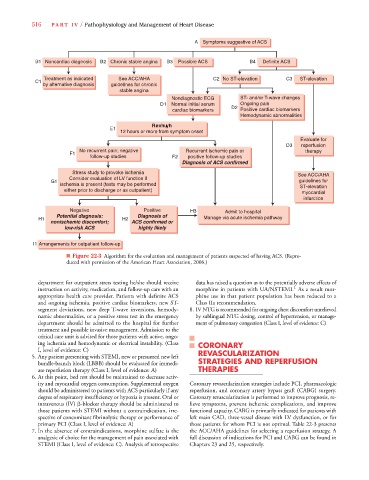
A Symptoms suggestive of ACS
B1 Noncardiac diagnosis B2 Chronic stable angina B3 Possible ACS B4 Definite ACS
Treatment as indicated See ACC/AHA C2 No ST-elevation C C3 ST-elevation
C1
by alternative diagnosis guidelines for chronic
stable angina
Nondiagnostic ECG ST- and/or T-wave changes
D1 Normal initial serum Ongoing pain
cardiac biomarkers D2 Positive cardiac biomarkers
Hemodynamic abnormalities
Revhuyh
E1
12 hours or more from symptom onset
Evaluate for
D3 reperfusion
No recurrent pain; negative Recurrent ischemic pain or therapy
F1
follow-up studies F2 positive follow-up studies
Diagnosis of ACS confirmed
Stress study to provoke ischemia See ACC/AHA
Consider evaluation of LV function if
G1 guidelines for
ischemia is present (tests may be performed ST-elevation
either prior to discharge or as outpatient)
myocardial
infarction
Negative Positive H3 Admit to hospital
Potential diagnosis: Diagnosis of
H1 H2 Manage via acute ischemia pathway
nonischemic discomfort; ACS confirmed or
low-risk ACS highly likely
I1 Arrangements for outpatient follow-up
■ Figure 22-3 Algorithm for the evaluation and management of patients suspected of having ACS. (Repro-
duced with permission of the American Heart Association, 2006.)
department for outpatient stress testing he/she should receive data has raised a question as to the potentially adverse effects of
1
instruction on activity, medication, and follow-up care with an morphine in patients with UA/NSTEMI. As a result mor-
appropriate health care provider. Patients with definite ACS phine use in that patient population has been reduced to a
and ongoing ischemia, positive cardiac biomarkers, new ST- Class IIa recommendation.
segment deviations, new deep T-wave inversions, hemody- 8. IV NTG is recommended for ongoing chest discomfort unrelieved
namic abnormalities, or a positive stress test in the emergency by sublingual NTG dosing, control of hypertension, or manage-
department should be admitted to the hospital for further ment of pulmonary congestion (Class I, level of evidence: C)
treatment and possible invasive management. Admission to the
critical care unit is advised for those patients with active, ongo-
ing ischemia and hemodynamic or electrical instability. (Class CORONARY
I, level of evidence: C) REVASCULARIZATION
5. Any patient presenting with STEMI, new or presumed new left
bundle-branch block (LBBB) should be evaluated for immedi- STRATEGIES AND REPERFUSION
ate reperfusion therapy (Class I, level of evidence: A) THERAPIES
6. At this point, bed rest should be maintained to decrease activ-
ity and myocardial oxygen consumption. Supplemental oxygen Coronary revascularization strategies include PCI, pharmacologic
should be administered to patients with ACS particularly if any reperfusion, and coronary artery bypass graft (CABG) surgery.
degree of respiratory insufficiency or hypoxia is present. Oral or Coronary revascularization is performed to improve prognosis, re-
intravenous (IV) -blocker therapy should be administered to lieve symptoms, prevent ischemic complications, and improve
those patients with STEMI without a contraindication, irre- functional capacity. CABG is primarily indicated for patients with
spective of concomitant fibrinolytic therapy or performance of left main CAD, three-vessel disease with LV dysfunction, or for
primary PCI (Class I, level of evidence: A) those patients for whom PCI is not optimal. Table 22-3 presents
7. In the absence of contraindications, morphine sulfate is the the ACC/AHA guidelines for selecting a reperfusion strategy. A
analgesic of choice for the management of pain associated with full discussion of indications for PCI and CABG can be found in
STEMI (Class I, level of evidence: C). Analysis of retrospective Chapters 23 and 25, respectively.