Page 602 - Cardiac Nursing
P. 602
M
3 P
M
Pa
Pa
55
3 P
55
p
p
g
A
78
A
p
p
g
g
e 5
78
e 5
1:4
6/2
6/2
0/0
3
0/0
0
1:4
0
009
009
3
94.
q
94.
5-5
5-5
xd
3
xd
q
q
K34
K34
LWB
0-c
24_
24_
0-c
t
t
p
ara
LWB
LWBK340-c24_ pp555-594.qxd 30/06/2009 01:43 PM Page 578 Aptara
ara
578 PA R T I V / Pathophysiology and Management of Heart Disease
Medications. Important advances have been made in the
pharmacologic treatment of patients with HF. But, there are MYOCARDIAL DYSFUNCTION
clearly many barriers to medication adherence in patients with
SYSTOLIC DIASTOLIC
HF. Common sense tells us that if patients are unable to obtain
medications or to take their medications correctly, the favorable
outcomes observed in clinical trails will not be seen clinically. LVEDP
Medication nonadherence is highly prevalent in patients with Cardiac output Pulmonary congestion
HF. 143,185,186 However, a positive association between patients’ Stroke volume
perception of the effects of a medication and subsequent adher-
ence has been demonstrated. 187 Education and support have like-
wise been shown to significantly increase adherence resulting in
improvements in functional outcome and reduced emergency Systemic Hypotension
perfusion
room visits and hospitalization. 188,189
Social Support and Quality of Life. There is evidence that Coronary Hypoxemia
a relationship between social support and health outcomes in pa- perfusion
tients with HF exists. Feldman et al. 144 evaluated the impact of pressure
sending e-mail reminders regarding HF-specific clinical recom-
mendations to home health nurses. Patients cared for by nurses re-
ceiving the prompts were significantly more likely to recognize Compensatory ISCHEMIA
their medications, less likely to report salting their food, and more vasoconstriction;
likely to weigh themselves. The Kansas City Cardiomyopathy fluid retention
Questionnaire score and health-related quality of life were signifi- PROGRESSIVE
MYOCARDIAL
cantly higher in the patients receiving care from a nurse receiving DYSFUNCTION
the prompts. This study is of interest, as it attempts to demonstrate
and measure the link between self-care practice and functional out-
comes. Was the improvement in outcome related to improved DEATH
knowledge and adherence or augmented provider patient interac-
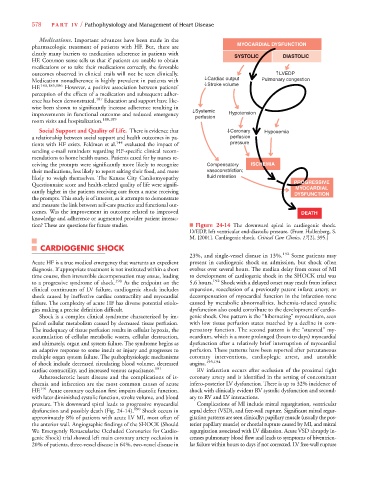
tion? These are questions for future studies. ■ Figure 24-14 The downward spiral in cardiogenic shock.
LVEDP, left ventricular end-diastolic pressure. (From Hollenberg, S.
M. [2001]. Cardiogenic shock. Critical Care Clinics, 17[2], 395.)
CARDIOGENIC SHOCK
23%, and single-vessel disease in 13%. 192 Some patients may
Acute HF is a true medical emergency that warrants an expedient present in cardiogenic shock on admission, but shock often
diagnosis. If appropriate treatment is not instituted within a short evolves over several hours. The median delay from onset of MI
time course, then irreversible decompensation may ensue, leading to development of cardiogenic shock in the SHOCK trial was
to a progressive syndrome of shock. 190 As the endpoint on the 5.6 hours. 192 Shock with a delayed onset may result from infarct
clinical continuum of LV failure, cardiogenic shock includes expansion, reocclusion of a previously patent infarct artery, or
shock caused by ineffective cardiac contractility and myocardial decompensation of myocardial function in the infarction zone
failure. The complexity of acute HF has diverse potential etiolo- caused by metabolic abnormalities. Ischemia-related systolic
gies making a precise definition difficult. dysfunction also could contribute to the development of cardio-
Shock is a complex clinical syndrome characterized by im- genic shock. One pattern is the “hibernating” myocardium, seen
paired cellular metabolism caused by decreased tissue perfusion. with low tissue perfusion states matched by a decline in com-
The inadequacy of tissue perfusion results in cellular hypoxia, the pensatory function. The second pattern is the “stunned” my-
accumulation of cellular metabolic wastes, cellular destruction, ocardium, which is a more prolonged (hours to days) myocardial
and ultimately, organ and system failure. The syndrome begins as dysfunction after a relatively brief interruption of myocardial
an adaptive response to some insult or injury and progresses to perfusion. These patterns have been reported after percutaneous
multiple organ system failure. The pathophysiologic mechanisms coronary interventions, cardioplegic arrest, and unstable
of shock include decreased circulating blood volume, decreased angina. 193,194
cardiac contractility, and increased venous capacitance. 191 RV infarction occurs after occlusion of the proximal right
Atherosclerotic heart disease and the complications of is- coronary artery and is identified in the setting of concomitant
chemia and infarction are the most common causes of acute infero-posterior LV dysfunction. There is up to 32% incidence of
HF. 191 Acute coronary occlusion first impairs diastolic function, shock with clinically evident RV systolic dysfunction and second-
with later diminished systolic function, stroke volume, and blood ary to RV and LV interactions.
pressure. This downward spiral leads to progressive myocardial Complications of MI include mitral regurgitation, ventricular
dysfunction and possibly death (Fig. 24-14). 190 Shock occurs in septal defect (VSD), and free-wall rupture. Significant mitral regur-
approximately 8% of patients with acute LV MI, most often of gitation patterns are seen clinically: papillary muscle (usually the pos-
the anterior wall. Angiographic findings of the SHOCK (Should terior papillary muscle) or chordal rupture caused by MI, and mitral
We Emergently Revascularize Occluded Coronaries for Cardio- regurgitation associated with LV dilatation. Acute VSD abruptly in-
genic Shock) trial showed left main coronary artery occlusion in creases pulmonary blood flow and leads to symptoms of biventricu-
20% of patients, three-vessel disease in 64%, two-vessel disease in lar failure within hours to days if not corrected. LV free-wall rupture