Page 718 - Cardiac Nursing
P. 718
09
/1/
49
P
AM
5-7
p65
04.
7
qxd
g
K34
0-c
LWBK340-c28_p655-704.qxd 7/1/09 9:9:49 AM Page 694 Aptara
LWB K34 0-c 28_ p65 5-7 04. qxd 7 /1/ 09 9: 49 AM P a a g e e 694 Ap tar a a
LWB
Ap
694
tar
28_
694 PA R T I V / Pathophysiology and Management Disease
2 2 2 2 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 2 2 2 2 3 3 3 3 2 2 2 2 3 3 3 3 2 2 2 2 5 5 5 5 5 5 5 5 5 2 2 2 2 8 8 8 8 0 0 0 0 5 5 5 5 2 2 2 2 4 4 4 4 4
8 8 8 9 9 9 4 4 4 5 5 5 5 5 5 4 4 4 5 5 5 4 4 4 5 5 5 5 5 5 5 5 5 4 4 4 5 5 5 4 4 4 5 5 5 3 3 3 3 2 2 2 5 5 5 9 9 9 0 0 0 1 1 5 5 5 8 8 8 8
0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0
A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A A
R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R b b b S S S R R R S S S S S S S S S S S S S S S S S R R R R R R
F F F F F F F F F F F F F F F F F F F F F F F F F F F T T T T T T T T T T T T F F F T T T T T T T T T T T T T T T T T T T T T T T T V V V V V V V V V V V V
S S S S S S S S S S S S S S S S S S S S S S S S S S S S S F F F F F F F F F F F F D D D P P P P P P P P P P P P P P P P P P P P P P P P P P P 8 8 8 8 8 8 8 8 8
2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 3 3 3 3 3 3 3 3 3 3 3 3 0 0 0 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 6 6 6 6 6 6 4 4 4 3 3 3
5 5 5 7 7 7 0 0 0 0 3 3 3 9 9 9 9 9 9 9 9 9 9 9 9 9 9 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 6 6 6 6 6 6 6 6 6 6 6 6 6 6 6 6 6 6 6 6 6 6 6 6 2 2 2 7 7 7 3 3 3 2 2 2
0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0
1
D
Defib
VF Rx 1 Defibb
VF
Rx
VF F VF Rx x 1 Def
V V
VF
g
h
g
V V F R 1 B r ust Du rin g g C har gin g
VF Rx 1 Brust During Charging
VF Rx 1 Brust Dur
u
Rx
i
ng Charging
R
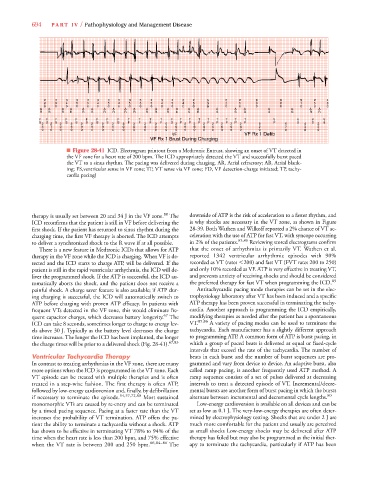
■ Figure 28-41 ICD. Electrogram printout from a Medtronic Entrust, showing an onset of VT detected in
the VF zone for a heart rate of 200 bpm. The ICD appropriately detected the VT and successfully burst paced
the VT to a sinus rhythm. The pacing was delivered during charging. AR, Atrial refractory; AB, Atrial blank-
ing; FS,ventricular sense in VF zone; TF, VT sense via VF zone; FD, VF detection-charge initiated; TP, tachy-
cardia pacing)
80
therapy is usually set between 20 and 34 J in the VF zone. The downside of ATP is the risk of acceleration to a faster rhythm, and
ICD reconfirms that the patient is still in VF before delivering the is why shocks are necessary in the VT zone, as shown in Figure
first shock. If the patient has returned to sinus rhythm during the 28-39. Both Wathen and Wilkoff reported a 2% chance of VT ac-
charging time, the first VF therapy is aborted. The ICD attempts celeration with the use of ATP for fast VT, with syncope occurring
to deliver a synchronized shock to the R wave if at all possible. in 2% of the patients. 85,86 Reviewing stored electrograms confirm
There is a new feature in Medtronic ICDs that allows for ATP that the onset of arrhythmias is primarily VT. Wathen et al.
therapy in the VF zone while the ICD is charging. When VF is de- reported 1342 ventricular arrhythmic episodes with 90%
tected and the ICD starts to charge ATP, will be delivered. If the recorded as VT (rates 200) and fast VT (FVT rates 200 to 250)
patient is still in the rapid ventricular arrhythmia, the ICD will de- and only 10% recorded as VF. ATP is very effective in treating VT,
liver the programmed shock. If the ATP is successful, the ICD au- and prevents anxiety of receiving shocks and should be considered
tomatically aborts the shock, and the patient does not receive a the preferred therapy for fast VT when programming the ICD. 85
painful shock. A charge saver feature is also available; if ATP dur- Antitachycardic pacing mode therapies can be set in the elec-
ing charging is successful, the ICD will automatically switch to trophysiology laboratory after VT has been induced and a specific
ATP before charging with proven ATP efficacy. In patients with ATP therapy has been proven successful in terminating the tachy-
frequent VTs detected in the VF zone, this would eliminate fre- cardia. Another approach is programming the ICD empirically,
quent capacitor charges, which decreases battery longevity. 67 The modifying therapies as needed after the patient has a spontaneous
ICD can take 8 seconds, sometimes longer to charge to energy lev- VT. 85,86 A variety of pacing modes can be used to terminate the
els above 30 J. Typically as the battery level decreases the charge tachycardia. Each manufacturer has a slightly different approach
time increases. The longer the ICD has been implanted, the longer to programming ATP. A common form of ATP is burst pacing, in
the charge times will be prior to a delivered shock (Fig. 28-41). 67,83 which a group of paced beats is delivered at equal or fixed-cycle
intervals that exceed the rate of the tachycardia. The number of
Ventricular Tachycardia Therapy beats in each burst and the number of burst sequences are pro-
In contrast to treating arrhythmias in the VF zone, there are many grammed and vary from device to device. An adaptive burst, also
more options when the ICD is programmed in the VT zone. Each called ramp pacing, is another frequently used ATP method. A
VT episode can be treated with multiple therapies and is often ramp sequence consists of a set of pulses delivered at decreasing
treated in a step-wise fashion. The first therapy is often ATP, intervals to treat a detected episode of VT. Incremental/decre-
followed by low-energy cardioversion and, finally, by defibrillation mental bursts are another form of burst pacing in which the bursts
if necessary to terminate the episode. 54,57,72,80 Most sustained alternate between incremental and decremental cycle lengths. 80
monomorphic VTs are caused by re-entry and can be terminated Low-energy cardioversion is available on all devices and can be
by a timed pacing sequence. Pacing at a faster rate than the VT set as low as 0.1 J. The very-low-energy therapies are often deter-
increases the probability of VT termination. ATP offers the pa- mined by electrophysiology testing. Shocks that are under 2 J are
tient the ability to terminate a tachycardia without a shock. ATP much more comfortable for the patient and usually are perceived
has shown to be effective in terminating VT 78% to 94% of the as small shocks Low-energy shocks may be delivered after ATP
time when the heart rate is less than 200 bpm, and 75% effective therapy has failed but may also be programmed as the initial ther-
when the VT rate is between 200 and 250 bpm. 66,84–86 The apy to terminate the tachycardia, particularly if ATP has been