Page 296 - ACCCN's Critical Care Nursing
P. 296
Cardiac Rhythm Assessment and Management 273
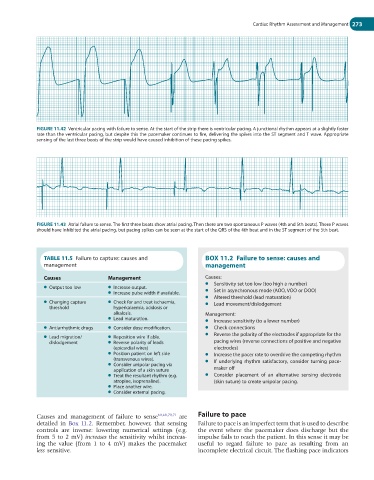
FIGURE 11.42 Ventricular pacing with failure to sense. At the start of the strip there is ventricular pacing. A junctional rhythm appears at a slightly faster
rate than the ventricular pacing, but despite this the pacemaker continues to fire, delivering the spikes into the ST segment and T wave. Appropriate
sensing of the last three beats of the strip would have caused inhibition of these pacing spikes.
FIGURE 11.43 Atrial failure to sense. The first three beats show atrial pacing. Then there are two spontaneous P waves (4th and 5th beats). These P waves
should have inhibited the atrial pacing, but pacing spikes can be seen at the start of the QRS of the 4th beat and in the ST segment of the 5th beat.
TABLE 11.5 Failure to capture: causes and BOX 11.2 Failure to sense: causes and
management management
Causes Management Causes:
● Sensitivity set too low (too high a number)
● Output too low ● Increase output.
● Increase pulse width if available. ● Set in asynchronous mode (AOO, VOO or DOO)
● Altered threshold (lead maturation)
● Changing capture ● Check for and treat ischaemia, ● Lead movement/dislodgement
threshold hyperkalaemia, acidosis or
alkalosis. Management:
● Lead maturation.
● Increase sensitivity (to a lower number)
● Antiarrhythmic drugs ● Consider dose modification. ● Check connections
● Reverse the polarity of the electrodes if appropriate for the
● Lead migration/ ● Reposition wire if able.
dislodgement ● Reverse polarity of leads pacing wires (reverse connections of positive and negative
(epicardial wires) electrodes)
● Position patient on left side ● Increase the pacer rate to overdrive the competing rhythm
(transvenous wires). ● If underlying rhythm satisfactory, consider turning pace-
● Consider unipolar pacing via
application of a skin suture maker off
● Treat the resultant rhythm (e.g. ● Consider placement of an alternative sensing electrode
atropine, isoprenaline). (skin suture) to create unipolar pacing.
● Place another wire.
● Consider external pacing.
Causes and management of failure to sense 60,68,70,71 are Failure to pace
detailed in Box 11.2. Remember, however, that sensing Failure to pace is an imperfect term that is used to describe
controls are inverse: lowering numerical settings (e.g. the event where the pacemaker does discharge but the
from 5 to 2 mV) increases the sensitivity whilst increas- impulse fails to reach the patient. In this sense it may be
ing the value (from 1 to 4 mV) makes the pacemaker useful to regard failure to pace as resulting from an
less sensitive. incomplete electrical circuit. The flashing pace indicators