Page 297 - ACCCN's Critical Care Nursing
P. 297
274 P R I N C I P L E S A N D P R A C T I C E O F C R I T I C A L C A R E
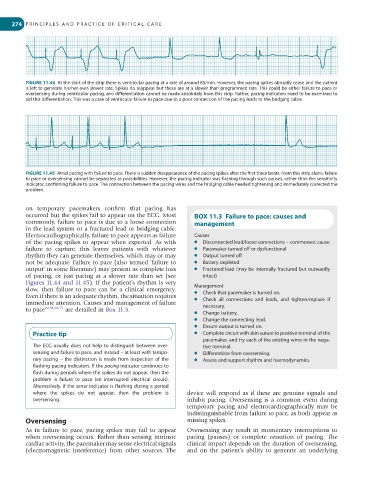
FIGURE 11.44 At the start of the strip there is ventricular pacing at a rate of around 85/min. However, the pacing spikes abruptly cease and the patient
is left to generate his/her own slower rate. Spikes do reappear but these are at a slower than programmed rate. This could be either failure to pace or
oversensing during ventricular pacing, and differentiation cannot be made absolutely from this strip. Rather, pacing indicators need to be examined to
aid this differentiation. This was a case of ventricular failure to pace due to a poor connection of the pacing leads to the bridging cable.
FIGURE 11.45 Atrial pacing with failure to pace. There is sudden disappearance of the pacing spikes after the first three beats. From this strip alone, failure
to pace or oversensing cannot be separated as possibilities. However, the pacing indicator was flashing through such pauses, rather than the sensitivity
indicator, confirming failure to pace. The connection between the pacing wires and the bridging cable needed tightening and immediately corrected the
problem.
on temporary pacemakers confirm that pacing has
occurred but the spikes fail to appear on the ECG. Most BOX 11.3 Failure to pace: causes and
commonly, failure to pace is due to a loose connection management
in the lead system or a fractured lead or bridging cable.
Electrocardiographically, failure to pace appears as failure Causes
of the pacing spikes to appear when expected. As with ● Disconnected lead/loose connections – commonest cause
failure to capture, this leaves patients with whatever ● Pacemaker turned off or dysfunctional
rhythm they can generate themselves, which may or may ● Output turned off
not be adequate. Failure to pace (also termed ‘failure to ● Battery depleted
output’ in some literature) may present as complete loss ● Fractured lead (may be internally fractured but outwardly
of pacing, or just pacing at a slower rate than set (see intact)
Figures 11.44 and 11.45). If the patient’s rhythm is very
slow, then failure to pace can be a clinical emergency. Management
Even if there is an adequate rhythm, the situation requires ● Check that pacemaker is turned on.
immediate attention. Causes and management of failure ● Check all connections and leads, and tighten/replace if
to pace 22,51,68-71 are detailed in Box 11.3. necessary.
● Change battery.
● Change the connecting lead.
● Ensure output is turned on.
Practice tip ● Complete circuit with skin suture to positive terminal of the
pacemaker, and try each of the existing wires in the nega-
The ECG usually does not help to distinguish between over- tive terminal.
sensing and failure to pace, and instead – at least with tempo- ● Differentiate from oversensing.
rary pacing – the distinction is made from inspection of the ● Assess and support rhythm and haemodynamics.
flashing pacing indicators. If the pacing indicator continues to
flash during periods where the spikes do not appear, then the
problem is failure to pace (an interrupted electrical circuit).
Alternatively, if the sense indicator is flashing during a period
where the spikes do not appear, then the problem is device will respond as if these are genuine signals and
oversensing. inhibit pacing. Oversensing is a common event during
temporary pacing and electrocardiographically may be
indistinguishable from failure to pace, as both appear as
Oversensing missing spikes.
As in failure to pace, pacing spikes may fail to appear Oversensing may result in momentary interruptions to
when oversensing occurs. Rather than sensing intrinsic pacing (pauses) or complete cessation of pacing. The
cardiac activity, the pacemaker may sense electrical signals clinical impact depends on the duration of oversensing,
(electromagnetic interference) from other sources. The and on the patient’s ability to generate an underlying