Page 356 - ACCCN's Critical Care Nursing
P. 356
Respiratory Assessment and Monitoring 333
Apex bicarbonate and pH returns to normal (i.e. the respiratory
Alveolus 11
Zone I alkalosis is compensated).
Capillary
Arteriole PA . Pa . Pv
Venule
PATHOPHYSIOLOGY
Three common pathophysiological concepts that influ-
Zone II ence respiratory function in critically ill patients are
Alveolus Pa . PA . Pv hypoxaemia, inflammation and oedema. The principles
for these phenomena are discussed below. Related pre-
Pulmonary Pulmonary senting disease states including respiratory failure, pneu-
artery vein
monia, acute lung injury, asthma and chronic obstructive
pulmonary disease are described in Chapter 14.
Alveolus
Zone III HYPOXAEMIA
Pa . Pv . PA
Hypoxaemia describes a decrease in the partial pressure
4
of oxygen in arterial blood (PaO 2 ) of less than 60 mmHg.
This state leads to less efficient anaerobic metabolism at
the tissue and end-organ level, and resulting compro-
mised cellular function. Hypoxia is abnormally low PO 2
in the tissues, and can be due to:
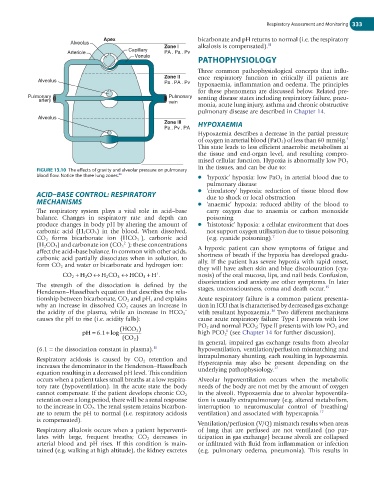
FIGURE 13.10 The effects of gravity and alveolar pressure on pulmonary
86
blood flow. Notice the three lung zones. ● ‘hypoxic’ hypoxia: low PaO 2 in arterial blood due to
pulmonary disease
ACID–BASE CONTROL: RESPIRATORY ● ‘circulatory’ hypoxia: reduction of tissue blood flow
due to shock or local obstruction
MECHANISMS ● ‘anaemic’ hypoxia: reduced ability of the blood to
The respiratory system plays a vital role in acid–base carry oxygen due to anaemia or carbon monoxide
balance. Changes in respiratory rate and depth can poisoning
produce changes in body pH by altering the amount of ● ‘histotoxic’ hypoxia: a cellular environment that does
carbonic acid (H 2 CO 3 ) in the blood. When dissolved, not support oxygen utilisation due to tissue poisoning
−
CO 2 forms bicarbonate ion (HCO 3 ), carbonic acid (e.g. cyanide poisoning). 7
2−
(H 2 CO 3 ) and carbonate ion (CO 3 ); these concentrations
affect the acid–base balance. In common with other acids, A hypoxic patient can show symptoms of fatigue and
carbonic acid partially dissociates when in solution, to shortness of breath if the hypoxia has developed gradu-
form CO 2 and water or bicarbonate and hydrogen ion: ally. If the patient has severe hypoxia with rapid onset,
they will have ashen skin and blue discolouration (cya-
CO 2 + H O ↔ H CO 3 ↔ HCO 3 + H . nosis) of the oral mucosa, lips, and nail beds. Confusion,
+
2
2
disorientation and anxiety are other symptoms. In later
The strength of the dissociation is defined by the 15
Henderson–Hasselbach equation that describes the rela- stages, unconsciousness, coma and death occur.
tionship between bicarbonate, CO 2 and pH, and explains Acute respiratory failure is a common patient presenta-
why an increase in dissolved CO 2 causes an increase in tion in ICU that is characterised by decreased gas exchange
−
16
the acidity of the plasma, while an increase in HCO 3 with resultant hypoxaemia. Two different mechanisms
causes the pH to rise (i.e. acidity falls): cause acute respiratory failure: Type I presents with low
PO 2 and normal PCO 2 ; Type II presents with low PO 2 and
( HCO 3 )
1
+
pH = 6 1 log high PCO 2 (see Chapter 14 for further discussion).
.
( CO 2 )
In general, impaired gas exchange results from alveolar
(6.1 = the dissociation constant in plasma). 11 hypoventilation, ventilation/perfusion mismatching and
intrapulmonary shunting, each resulting in hypoxaemia.
Respiratory acidosis is caused by CO 2 retention and
increases the denominator in the Henderson–Hasselbach Hypercapnia may also be present depending on the
17
equation resulting in a decreased pH level. This condition underlying pathophysiology.
occurs when a patient takes small breaths at a low respira- Alveolar hypoventilation occurs when the metabolic
tory rate (hypoventilation). In the acute state the body needs of the body are not met by the amount of oxygen
cannot compensate. If the patient develops chronic CO 2 in the alveoli. Hypoxaemia due to alveolar hypoventila-
retention over a long period, there will be a renal response tion is usually extrapulmonary (e.g. altered metabolism,
to the increase in CO 2 . The renal system retains bicarbon- interruption to neuromuscular control of breathing/
ate to return the pH to normal (i.e. respiratory acidosis ventilation) and associated with hypercapnia. 17
is compensated).
Ventilation/perfusion (V/Q) mismatch results when areas
Respiratory alkalosis occurs when a patient hyperventi- of lung that are perfused are not ventilated (no par-
lates with large, frequent breaths; CO 2 decreases in ticipation in gas exchange) because alveoli are collapsed
arterial blood and pH rises. If this condition is main- or infiltrated with fluid from inflammation or infection
tained (e.g. walking at high altitude), the kidney excretes (e.g. pulmonary oedema, pneumonia). This results in