Page 393 - ACCCN's Critical Care Nursing
P. 393
370 P R I N C I P L E S A N D P R A C T I C E O F C R I T I C A L C A R E
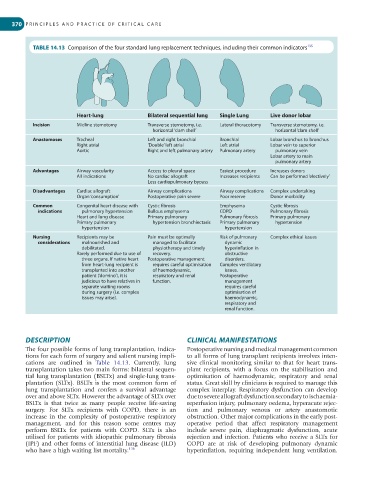
TABLE 14.13 Comparison of the four standard lung replacement techniques, including their common indicators 135
Heart-lung Bilateral sequential lung Single Lung Live donor lobar
Incision Midline sternotomy Transverse sternotomy, i.e. Lateral thoracotomy Transverse sternotomy, i.e.
horizontal ‘clam shell’ horizontal ‘clam shell’
Anastomoses Tracheal Left and right bronchial Bronchial Lobar bronchus to bronchus
Right atrial ’Double’ left atrial Left atrial Lobar vein to superior
Aortic Right and left pulmonary artery Pulmonary artery pulmonary vein
Lobar artery to main
pulmonary artery
Advantages Airway vascularity Access to pleural space Easiest procedure Increases donors
All indications No cardiac allograft Increases recipients Can be performed ‘electively’
Less cardiopulmonary bypass
Disadvantages Cardiac allograft Airway complications Airway complications Complex undertaking
Organ ‘consumption’ Postoperative pain severe Poor reserve Donor morbidity
Common Congenital heart disease with Cystic fibrosis Emphysema Cystic fibrosis
indications pulmonary hypertension Bullous emphysema COPD Pulmonary fibrosis
Heart and lung disease Primary pulmonary Pulmonary fibrosis Primary pulmonary
Primary pulmonary hypertension bronchiectasis Primary pulmonary hypertension
hypertension hypertension
Nursing Recipients may be Pain must be optimally Risk of pulmonary Complex ethical issues
considerations malnourished and managed to facilitate dynamic
debilitated. physiotherapy and timely hyperinflation in
Rarely performed due to use of recovery. obstructive
three organs. If native heart Postoperative management disorders.
from heart-lung recipient is requires careful optimisation Complex ventilatory
transplanted into another of haemodynamic, issues.
patient (’domino’), it is respiratory and renal Postoperative
judicious to have relatives in function. management
separate waiting rooms requires careful
during surgery (i.e. complex optimisation of
issues may arise). haemodynamic,
respiratory and
renal function.
DESCRIPTION CLINICAL MANIFESTATIONS
The four possible forms of lung transplantation, indica- Postoperative nursing and medical management common
tions for each form of surgery and salient nursing impli- to all forms of lung transplant recipients involves inten-
cations are outlined in Table 14.13. Currently, lung sive clinical monitoring similar to that for heart trans-
transplantation takes two main forms: bilateral sequen- plant recipients, with a focus on the stabilisation and
tial lung transplantation (BSLTx) and single-lung trans- optimisation of haemodynamic, respiratory and renal
plantation (SLTx). BSLTx is the most common form of status. Great skill by clinicians is required to manage this
lung transplantation and confers a survival advantage complex interplay. Respiratory dysfunction can develop
over and above SLTx. However the advantage of SLTx over due to severe allograft dysfunction secondary to ischaemia-
BSLTx is that twice as many people receive life-saving reperfusion injury, pulmonary oedema, hyperacute rejec-
surgery. For SLTx recipients with COPD, there is an tion and pulmonary venous or artery anastomotic
increase in the complexity of postoperative respiratory obstruction. Other major complications in the early post-
management, and for this reason some centres may operative period that affect respiratory management
perform BSLTx for patients with COPD. SLTx is also include severe pain, diaphragmatic dysfunction, acute
utilised for patients with idiopathic pulmonary fibrosis rejection and infection. Patients who receive a SLTx for
(IPF) and other forms of interstitial lung disease (ILD) COPD are at risk of developing pulmonary dynamic
who have a high waiting list mortality. 136 hyperinflation, requiring independent lung ventilation.