Page 389 - ACCCN's Critical Care Nursing
P. 389
366 P R I N C I P L E S A N D P R A C T I C E O F C R I T I C A L C A R E
Ventilatory Limitation
Increased Ventitatory Requirement
Increased Work of Breathing
Deconditioning
LV Dysfunction Reduced
Pulmonary
Conductance
O 2
CO 2
• •
QO 2
CO 2 O 2 VCO 2
MUSCLE SYSTEMIC PULMONARY LUNGS
(Lactic Acidosis) CIRCULATION CIRCULATION
• O 2 CO 2
QCO 2 CO 2 •
VO 2
O 2
RV Dysfunction
Loss of
Gas Exchanging
Surface Area
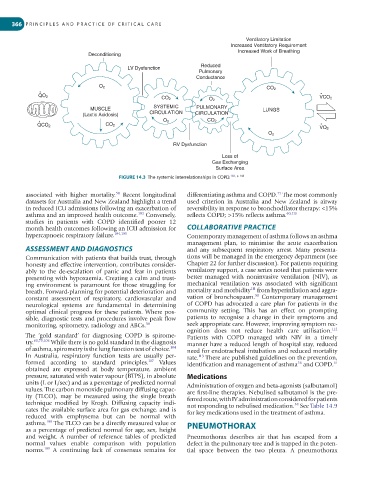
FIGURE 14.3 The systemic interrelationships in COPD. 102, p. 148
58
71
associated with higher mortality. Recent longitudinal differentiating asthma and COPD. The most commonly
datasets for Australia and New Zealand highlight a trend used criterion in Australia and New Zealand is airway
in reduced ICU admissions following an exacerbation of reversibility in response to bronchodilator therapy: <15%
asthma and an improved health outcome. Conversely, reflects COPD; >15% reflects asthma. 60,110
103
studies in patients with COPD identified poorer 12
month health outcomes following an ICU admission for COLLABORATIVE PRACTICE
hypercapnoeic respiratory failure. 104,105 Contemporary management of asthma follows an asthma
management plan, to minimise the acute exacerbation
ASSESSMENT AND DIAGNOSTICS and any subsequent respiratory arrest. Many presenta-
Communication with patients that builds trust, through tions will be managed in the emergency department (see
honesty and effective intervention, contributes consider- Chapter 22 for further discussion). For patients requiring
ably to the de-escalation of panic and fear in patients ventilatory support, a case series noted that patients were
presenting with hypoxaemia. Creating a calm and trust- better managed with noninvasive ventilation (NIV), as
ing environment is paramount for those struggling for mechanical ventilation was associated with significant
111
breath. Forward-planning for potential deterioration and mortality and morbidity from hyperinflation and aggra-
58
constant assessment of respiratory, cardiovascular and vation of bronchospasm. Contemporary management
neurological systems are fundamental in determining of COPD has advocated a care plan for patients in the
optimal clinical progress for these patients. Where pos- community setting. This has an effect on prompting
sible, diagnostic tests and procedures involve peak flow patients to recognise a change in their symptoms and
monitoring, spirometry, radiology and ABGs. 58 seek appropriate care. However, improving symptom rec-
112
ognition does not reduce health care utilisation.
The ‘gold standard’ for diagnosing COPD is spirome- Patients with COPD managed with NIV in a timely
try. 60,75,106 While there is no gold standard in the diagnosis manner have a reduced length of hospital stay, reduced
of asthma, spirometry is the lung function test of choice. need for endotracheal intubation and reduced mortality
104
In Australia, respiratory function tests are usually per- rate. There are published guidelines on the prevention,
113
formed according to standard principles. Values identification and management of asthma and COPD. 61
107
56
obtained are expressed at body temperature, ambient
pressure, saturated with water vapour (BTPS), in absolute Medications
units (L or L/sec) and as a percentage of predicted normal Administration of oxygen and beta-agonists (salbutamol)
values. The carbon monoxide pulmonary diffusing capac- are first-line therapies. Nebulised salbutamol is the pre-
ity (TLCO), may be measured using the single breath ferred route, with IV administration considered for patients
technique modified by Krogh. Diffusing capacity indi- not responding to nebulised medication. See Table 14.9
58
cates the available surface area for gas exchange, and is for key medications used in the treatment of asthma.
reduced with emphysema but can be normal with
108
asthma. The TLCO can be a directly measured value or PNEUMOTHORAX
as a percentage of predicted normal for age, sex, height
and weight. A number of reference tables of predicted Pneumothorax describes air that has escaped from a
normal values enable comparison with population defect in the pulmonary tree and is trapped in the poten-
109
norms. A continuing lack of consensus remains for tial space between the two pleura. A pneumothorax