Page 1187 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 1187
Chapter 66 Acute Lymphoblastic Leukemia in Adults 1035
B-lymphoblastic leukemia/lymphoma cytoplasmic vacuolation and need to be distinguished from leukemic
presentation of Burkitt lymphoma (BL). Unlike ALL, BL cells are
mature B cells with bright surface Ig expression, very strong CD20
Flow cytometry including CRLF2, cytogenetics expression, and no expression of CD34. Diagnosis of BL is confirmed
by the presence of an MYC translocation using FISH or cytogenetics.
Other entities that require distinction from ALL depend on the age
of presentation. In the pediatric age group, ALL blasts need to be
Hyper/hypodiploid, Rearranged BCR-ABL1, MLL, distinguished from hematogones. Hematogones are normal B-cell
other B-ALL TCF3-PBX1 or ETV6-RUNX1 precursors present within the BM. These are more abundant in child-
hood and decrease with increasing age. Hematogones may also be
Not Ph-like increased during hematopoietic regeneration, particularly after che-
motherapy or BM engraftment after stem cell transplant. Hemato-
FISH for rearrangement: CRLF2 positive gones possess a distinct pattern of antigen expression that recapitulates
ABL1, ABL2, CSF1R, by flow progressive B-cell maturation. This is reflected in progressive loss of
JAK2, PDGFRB
antigens such as CD34, TdT, and CD10 and acquisition of CD20
Confirm by FISH and surface Ig expression (Fig. 66.6). Other diseases that need to be
morphologically distinguished from ALL include small blue cell
tumors, including Ewing sarcoma, neuroblastoma, and medulloblas-
Ph-like if rearrangement present toma. Ancillary studies, including immunophenotyping and cytoge-
netics, are helpful in making the distinction. In older adults, entities
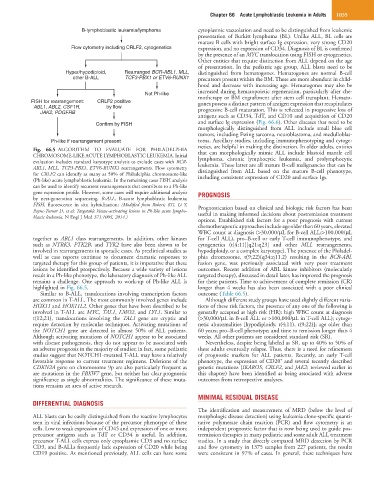
Fig. 66.5 ALGORITHM TO EVALUATE FOR PHILADELPHIA that can morphologically mimic ALL include blastoid mantle cell
CHROMOSOME-LIKE ACUTE LYMPHOBLASTIC LEUKEMIA. Initial lymphoma, chronic lymphocytic leukemia, and prolymphocytic
evaluation includes standard karyotype analysis to exclude cases with BCR- leukemia. These latter are all mature B-cell malignancies that can be
ABL1, MLL, TCF3-PBX1, ETV6-RUNX1 rearrangements. Flow cytometry distinguished from ALL based on the mature B-cell phenotype,
for CRLF2 can identify as many as 50% of Philadelphia chromosome-like including consistent expression of CD20 and surface Igs.
(Ph-like) acute lymphoblastic leukemia. In the remaining cases FISH analysis
can be used to identify recurrent rearrangements that contribute to a Ph-like
gene expression profile. However, some cases will require additional analysis PROGNOSIS
by next-generation sequencing. B-ALL, B-acute lymphoblastic leukemia;
FISH, fluorescence in situ hybridization; (Modified from Roberts KG, Li Y, Prognostication based on clinical and biologic risk factors has been
Payne-Turner D, et al: Targetable kinase-activating lesions in Ph-like acute lympho- useful in making informed decisions about postremission treatment
blastic leukemia. N Engl J Med 371:1005, 2014.)
options. Established risk factors for a poor prognosis with current
chemotherapeutic approaches include age older than 60 years, elevated
WBC count at diagnosis (>30,000/µL for B-cell ALL;>100,000/µL
together as ABL1 class rearrangements. In addition, other kinases for T-cell ALL), pro–B-cell or early T-cell immunophenotype, and
such as NTRK3, PTK2B, and TYK2 have also been shown to be cytogenetics (t[4;11][q21;q23] and other MLL rearrangements,
involved in rearrangements in sporadic cases. As preclinical studies as hypodiploidy, or a complex karyotype). The presence of the Philadel-
well as case reports continue to document dramatic responses to phia chromosome, t(9;22)(q34;q11.2) resulting in the BCR-ABL
targeted therapy for this group of patients, it is imperative that these fusion gene, was previously associated with very poor treatment
lesions be identified prospectively. Because a wide variety of lesions outcomes. Recent addition of ABL kinase inhibitors (molecularly
result in a Ph-like phenotype, the laboratory diagnosis of Ph-like ALL targeted therapy), discussed in detail later, has improved the prognosis
remains a challenge. One approach to work-up of Ph-like ALL is for these patients. Time to achievement of complete remission (CR)
highlighted in Fig. 66.5. longer than 4 weeks has also been associated with a poor clinical
Similar to B-ALL, translocations involving transcription factors outcome (Table 66.5).
are common in T-ALL. The most commonly involved genes include Although different study groups have used slightly different varia-
HOX11 and HOX11L2. Other genes that have been described to be tions of these risk factors, the presence of any one of the following is
involved in T-ALL are MYC, TAL1, LMO2, and LYL1. Similar to generally accepted as high risk (HR): high WBC count at diagnosis
t(12;21), translocations involving the TAL1 gene are cryptic and (>30,000/µL in B-cell ALL or >100,000/µL in T-cell ALL); cytoge-
require detection by molecular techniques. Activating mutations of netic abnormalities [hypodiploidy, t(4;11), t(9;22)]; age older than
the NOTCH1 gene are detected in almost 50% of ALL patients. 60 years; pro–B-cell phenotype; and time to remission longer than 4
Although activating mutations of NOTCH1 appear to be associated weeks. All other patients are considered standard risk (SR).
with disease pathogenesis, they do not appear to be associated with Nevertheless, despite being labeled as SR, up to 40% to 50% of
an adverse prognosis in the majority of studies; in fact, some pediatric these adults eventually relapse. Thus, there is a need for refinement
studies suggest that NOTCH1-mutated T-ALL may have a relatively of prognostic markers for ALL patients. Recently, an early T-cell
+
favorable response to current treatment regimens. Deletions of the phenotype, the expression of CD20 and several recently described
CDKN2A gene on chromosome 9p are also particularly frequent as genetic mutations (IKAROS, CRLF2, and JAK2; reviewed earlier in
are mutations in the FBXW7 gene, but neither has clear prognostic this chapter) have been identified as being associated with adverse
significance as single abnormalities. The significance of these muta- outcomes from retrospective analyses.
tions remains an area of active research.
MINIMAL RESIDUAL DISEASE
DIFFERENTIAL DIAGNOSIS
The identification and measurement of MRD (below the level of
ALL blasts can be easily distinguished from the reactive lymphocytes morphologic disease detection) using leukemia clone-specific quanti-
seen in viral infections because of the precursor phenotype of these tative polymerase chain reaction (PCR) and flow cytometry is an
cells. Low to weak expression of CD45 and expression of one or more independent prognostic factor that is now being used to guide pos-
precursor antigens such as TdT or CD34 is useful. In addition, tremission therapies in many pediatric and some adult ALL treatment
precursor T-ALL cells express only cytoplasmic CD3 and no surface studies. In a study that directly compared MRD detection by PCR
CD3, and B-ALLs frequently lack expression of CD20 while being and flow cytometry in 1375 samples from 227 patients, the results
CD19 positive. As mentioned previously, ALL cells can have some were consistent in 97% of cases. In general, these techniques have