Page 1329 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 1329
Chapter 72 Mast Cells and Mastocytosis 1175
Expected US survival compared to all systemic mastocytosis patients TABLE “C” Findings: Indication of Organ Damage Attributable
100 72.6 to Neoplastic Mast Cell Infiltration
Observed survival
Expected US survival 1. Cytopenia(s): Absolute neutrophil count <1000/µL or hemoglobin
80 <10 g/dL or platelets <100,000/µL
2. Hepatomegaly with ascites and/or impaired liver function
3. Palpable splenomegaly with hypersplenism
60
Survival 40 4. Malabsorption with hypoalbuminemia and weight loss
5. Skeletal lesions: large-sized osteolyses or severe osteoporosis
causing pathologic fractures
6. Life-threatening organopathy in other organ systems that is
20 definitively caused by an infiltration of the tissue by neoplastic mast
cells
0
0 10 20 30
A Years from Dx nuclei, metachromatic blasts, and mitotic figures. In MCL, circulat-
ing MCs (≥10% of nucleated cells) may be found; however, the
aleukemic MCL variant (<10% MCs in the peripheral blood) is more
common. MCL may arise de novo or progress from less advanced
forms of SM, such as ASM with elevated MC counts on the BM
Expected US Survival compared to WHO classification 13
aspirate. MCL typically has a dismal prognosis with a life expectancy
100 ISM, (n=159) of 6 months or less in most patients (see Fig. 72.1). 11,13,14 However,
ASM, (n=41) a chronic form of MCL has also been described, wherein patients
SM-AHN, (n=138) meet histopathologic criteria for the disease, but without C findings
80 MCL, (n=4) (see later). In these cases, MCs tend to show a more mature mor-
13
Expected US survival phology. However, even those with the initially more indolent form
60
Survival of (chronic) MCL are expected to show progression over time with
development of organ damage (transformation to acute MCL) and
limited survival.
40
MC sarcoma (MCS) is a rare MC tumor that can invade local
tissues and has a high potential to develop advanced systemic disease
20
with a fulminant course. In particular, most if not all patients with
MCS progress to MCL within a relatively short time period. Extra-
0 cutaneous mastocytoma is another rare SM variant that typically
follows a benign course.
0 10 20 30
Well-differentiated SM (WDSM) is a more recently described,
B Years from Dx rare variant of SM that is not yet formally recognized by the WHO
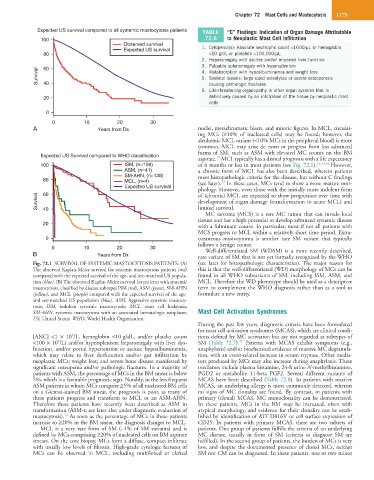
Fig. 72.1 SURVIVAL OF SYSTEMIC MASTOCYTOSIS PATIENTS. (A) (see later for histopathologic characteristics). The major reason for
The observed Kaplan-Meier survival for systemic mastocytosis patients (red) this is that the well-differentiated (WD) morphology of MCs can be
compared with the expected survival of the age- and sex-matched US popula- found in all WHO subvariants of SM, including ISM, ASM, and
tion (blue). (B) The observed Kaplan-Meier survival for patients with systemic MCL. Therefore the WD phenotype should be used as a descriptive
mastocytosis, classified by disease subtypes ISM (red), ASM (green), SM-AHN term to complement the WHO diagnosis rather than as a tool to
(yellow), and MCL (purple) compared with the expected survival of the age- formulate a new entity.
and sex-matched US population (blue). ASM, Aggressive systemic mastocy-
tosis; ISM, indolent systemic mastocytosis; MCL, mast cell leukemia;
SM-AHN, systemic mastocytosis with an associated hematologic neoplasm; Mast Cell Activation Syndromes
US, United States; WHO, World Health Organization.
During the past few years, diagnostic criteria have been formulated
for mast cell activation syndromes (MCAS), which are clinical condi-
9
[ANC] <1 × 10 /L, hemoglobin <10 g/dL, and/or platelet count tions defined by MC activation but are not regarded as subtypes of
15
9
<100 × 10 /L) and/or hypersplenism; hepatomegaly with liver dys- SM (Table 72.7). Patients with MCAS exhibit symptoms (e.g.,
function, and/or portal hypertension or ascites; hypoalbuminemia, anaphylaxis) and/or biochemical evidence of massive MC degranula-
which may relate to liver dysfunction and/or gut infiltration by tion, with an event-related increase in serum tryptase. Other media-
neoplastic MCs; weight loss; and severe bone disease manifested by tors produced by MCs may also increase during anaphylaxis. These
significant osteopenia and/or pathologic fractures. In a majority of mediators include plasma histamine, 24-h urine N-methylhistamine,
patients with ASM, the percentage of MCs in the BM smear is below PGD2 or metabolite 11-beta PGF2. Several different variants of
5%, which is a favorable prognostic sign. Notably, in the less frequent MCAS have been described (Table 72.8). In patients with reactive
ASM patients in whom MCs comprise ≥5% of all nucleated BM cells MCAS, an underlying allergy is most commonly detected, whereas
on a Giemsa-stained BM smear, the prognosis is poor, as many of no signs of MC clonality are found. By contrast, in patients with
these patients progress and transform to MCL or an ASM-AHN. primary (clonal) MCAS, MC monoclonality can be demonstrated.
Therefore these patients have recently been described as ASM in In these patients, MCs in the BM may be increased, often with
transformation (ASM-t; see later also under diagnostic evaluation of atypical morphology, and evidence for their clonality can be estab-
13
mastocytosis). As soon as the percentage of MCs in these patients lished by identification of KIT D816V or cell surface expression of
increase to ≥20% in the BM smear, the diagnosis changes to MCL. CD25. In patients with primary MCAS, there are two subsets of
MCL is a very rare form of SM (~1% of SM variants) and is patients. One group of patients fulfills the criteria of an underlying
defined by MCs comprising ≥20% of nucleated cells on BM aspirate MC disease, usually in form of SM (criteria to diagnose SM are
smears. On the core biopsy, MCs form a diffuse, compact infiltrate fulfilled). In the second group of patients, the burden of MCs is very
with usually low levels of fibrosis. High-grade cytologic features of low, and despite the documented presence of clonal MCs, neither
MCs can be observed in MCL, including multilobed or clefted SM nor CM can be diagnosed. In these patients, one or two minor