Page 2066 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 2066
Chapter 122 Overview of Hemostasis and Thrombosis 1835
Vascular Contact
injury activation
TF VIIa VIIIa H
Extrinsic IX X IXa VIIIa L IXa X Intrinsic
tenase tenase
Prothrombinase
Xa Va H Xa
Va L II
Xa
IIa
Fibrinogen Fibrin
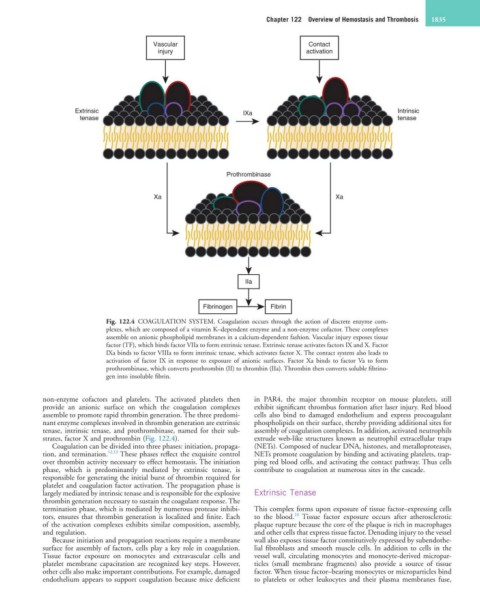
Fig. 122.4 COAGULATION SYSTEM. Coagulation occurs through the action of discrete enzyme com-
plexes, which are composed of a vitamin K–dependent enzyme and a non-enzyme cofactor. These complexes
assemble on anionic phospholipid membranes in a calcium-dependent fashion. Vascular injury exposes tissue
factor (TF), which binds factor VIIa to form extrinsic tenase. Extrinsic tenase activates factors IX and X. Factor
IXa binds to factor VIIIa to form intrinsic tenase, which activates factor X. The contact system also leads to
activation of factor IX in response to exposure of anionic surfaces. Factor Xa binds to factor Va to form
prothrombinase, which converts prothrombin (II) to thrombin (IIa). Thrombin then converts soluble fibrino-
gen into insoluble fibrin.
non-enzyme cofactors and platelets. The activated platelets then in PAR4, the major thrombin receptor on mouse platelets, still
provide an anionic surface on which the coagulation complexes exhibit significant thrombus formation after laser injury. Red blood
assemble to promote rapid thrombin generation. The three predomi- cells also bind to damaged endothelium and express procoagulant
nant enzyme complexes involved in thrombin generation are extrinsic phospholipids on their surface, thereby providing additional sites for
tenase, intrinsic tenase, and prothrombinase, named for their sub- assembly of coagulation complexes. In addition, activated neutrophils
strates, factor X and prothrombin (Fig. 122.4). extrude web-like structures known as neutrophil extracellular traps
Coagulation can be divided into three phases: initiation, propaga- (NETs). Composed of nuclear DNA, histones, and metalloproteases,
tion, and termination. 12,13 These phases reflect the exquisite control NETs promote coagulation by binding and activating platelets, trap-
over thrombin activity necessary to effect hemostasis. The initiation ping red blood cells, and activating the contact pathway. Thus cells
phase, which is predominantly mediated by extrinsic tenase, is contribute to coagulation at numerous sites in the cascade.
responsible for generating the initial burst of thrombin required for
platelet and coagulation factor activation. The propagation phase is
largely mediated by intrinsic tenase and is responsible for the explosive Extrinsic Tenase
thrombin generation necessary to sustain the coagulant response. The
termination phase, which is mediated by numerous protease inhibi- This complex forms upon exposure of tissue factor–expressing cells
14
tors, ensures that thrombin generation is localized and finite. Each to the blood. Tissue factor exposure occurs after atherosclerotic
of the activation complexes exhibits similar composition, assembly, plaque rupture because the core of the plaque is rich in macrophages
and regulation. and other cells that express tissue factor. Denuding injury to the vessel
Because initiation and propagation reactions require a membrane wall also exposes tissue factor constitutively expressed by subendothe-
surface for assembly of factors, cells play a key role in coagulation. lial fibroblasts and smooth muscle cells. In addition to cells in the
Tissue factor exposure on monocytes and extravascular cells and vessel wall, circulating monocytes and monocyte-derived micropar-
platelet membrane capacitation are recognized key steps. However, ticles (small membrane fragments) also provide a source of tissue
other cells also make important contributions. For example, damaged factor. When tissue factor–bearing monocytes or microparticles bind
endothelium appears to support coagulation because mice deficient to platelets or other leukocytes and their plasma membranes fuse,