Page 2068 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 2068
Chapter 122 Overview of Hemostasis and Thrombosis 1837
inhibitors modulate coagulation: TFPI and antithrombin. TFPI,
K PK which is located on platelets and microvascular endothelial cells,
inhibits factor VIIa in a factor Xa-dependent manner. TFPI effectively
HK HK halts tissue factor-mediated initiation of coagulation, but not before
sufficient factor Xa is generated to propagate clotting. The high levels
of thrombin produced during the amplification phase are controlled
XII XIIa
Surface by antithrombin. This serine protease inhibitor (serpin) also inacti-
vates other coagulation proteases, including factors VIIa, IXa, Xa, and
Xia. Although antithrombin is abundant, it exhibits only moderate
inhibitory activity, except in the presence of cell-associated glycosami-
noglycans, such as heparan sulfate. This is the biochemical basis for
XI XIa use of heparin as an anticoagulant (see Chapter 149). Further regula-
tion of thrombin generation is mediated by the protein C anticoagu-
lant pathway which is catalyzed by thrombin. These processes ensure
IX IXa that thrombin generation is localized and limited. Sufficient thrombin
is produced, however, to ensure that coagulation occurs.
Common Fibrin Formation
Surface Pathway
Thrombin converts soluble fibrinogen into insoluble fibrin. Fibrino-
gen is a dimeric molecule, each half of which is composed of three
polypeptide chains, the Aα, Bβ, and γ chains. Numerous disulfide
Thrombin
bonds covalently link the chains together and join the two halves of
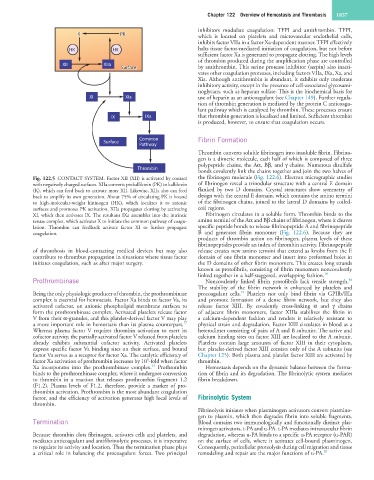
Fig. 122.5 CONTACT SYSTEM. Factor XII (XII) is activated by contact the fibrinogen molecule (Fig. 122.6). Electron micrographic studies
with negatively charged surfaces. XIIa converts prekallikrein (PK) to kallikrein of fibrinogen reveal a trinodular structure with a central E domain
(K), which can feed back to activate more XII. Likewise, XIIa also can feed flanked by two D domains. Crystal structures show symmetry of
back to amplify its own generation. About 75% of circulating PK is bound design with the central E domain, which contains the amino termini
to high-molecular-weight kininogen (HK), which localizes it to anionic of the fibrinogen chains, joined to the lateral D domains by coiled-
surfaces and promotes PK activation. XIIa propagates clotting by activating coil regions.
XI, which then activates IX. The resultant IXa assembles into the intrinsic Fibrinogen circulates in a soluble form. Thrombin binds to the
tenase complex, which activates X to initiate the common pathway of coagu- amino termini of the Aα and Bβ chains of fibrinogen, where it cleaves
lation. Thrombin can feedback activate factor XI to further propagate specific peptide bonds to release fibrinopeptide A and fibrinopeptide
coagulation. B and generates fibrin monomer (Fig. 122.6). Because they are
products of thrombin action on fibrinogen, plasma levels of these
fibrinopeptides provide an index of thrombin activity. Fibrinopeptide
of thrombosis in blood-contacting medical devices but may also release creates new amino termini that extend as knobs from the E
contribute to thrombus propagation in situations where tissue factor domain of one fibrin monomer and insert into preformed holes in
initiates coagulation, such as after major surgery. the D domains of other fibrin monomers. This creates long strands
known as protofibrils, consisting of fibrin monomers noncovalently
linked together in a half-staggered, overlapping fashion. 18
Prothrombinase Noncovalently linked fibrin protofibrils lack tensile strength.
18
The stability of the fibrin network is enhanced by platelets and
19
Being the only physiologic producer of thrombin, the prothrombinase procoagulant cells. Platelets not only bind fibrin via GPIIb/IIIa
complex is essential for hemostasis. Factor Xa binds to factor Va, its and promote formation of a dense fibrin network, but they also
activated cofactor, on anionic phospholipid membrane surfaces to release factor XIII. By covalently cross-linking α and γ chains
form the prothrombinase complex. Activated platelets release factor of adjacent fibrin monomers, factor XIIIa stabilizes the fibrin in
V from their α-granules, and this platelet-derived factor V may play a calcium-dependent fashion and renders it relatively resistant to
17
a more important role in hemostasis than its plasma counterpart. physical strain and degradation. Factor XIII circulates in blood as a
Whereas plasma factor V requires thrombin activation to exert its heterodimer consisting of pairs of A and B subunits. The active and
cofactor activity, the partially activated factor V released from platelets calcium binding sites on factor XIII are localized to the A subunit.
already exhibits substantial cofactor activity. Activated platelets Platelets contain large amounts of factor XIII in their cytoplasm,
express specific factor Va binding sites on their surface, and bound but platelet-derived factor XIII consists only of the A subunits (see
factor Va serves as a receptor for factor Xa. The catalytic efficiency of Chapter 125). Both plasma and platelet factor XIII are activated by
5
factor Xa activation of prothrombin increases by 10 -fold when factor thrombin.
13
Xa incorporates into the prothrombinase complex. Prothrombin Hemostasis depends on the dynamic balance between the forma-
binds to the prothrombinase complex, where it undergoes conversion tion of fibrin and its degradation. The fibrinolytic system mediates
to thrombin in a reaction that releases prothrombin fragment 1.2 fibrin breakdown.
(F1.2). Plasma levels of F1.2, therefore, provide a marker of pro-
thrombin activation. Prothrombin is the most abundant coagulation
factor, and the efficiency of activation generates high local levels of Fibrinolytic System
thrombin.
Fibrinolysis initiates when plasminogen activators convert plasmino-
gen to plasmin, which then degrades fibrin into soluble fragments.
Termination Blood contains two immunologically and functionally distinct plas-
minogen activators, t-PA and u-PA. t-PA mediates intravascular fibrin
Because thrombin clots fibrinogen, activates cells and platelets, and degradation, whereas u-PA binds to a specific u-PA receptor (u-PAR)
mediates anticoagulant and antifibrinolytic processes, it is imperative on the surface of cells, where it activates cell-bound plasminogen.
to regulate its activity and location. Thus the termination phase plays Consequently, pericellular proteolysis during cell migration and tissue
a critical role in balancing the procoagulant forces. Two principal remodeling and repair are the major functions of u-PA. 20