Page 1336 - Williams Hematology ( PDFDrive )
P. 1336
1310 Part X: Malignant Myeloid Diseases Chapter 85: Essential Thrombocythemia 1311
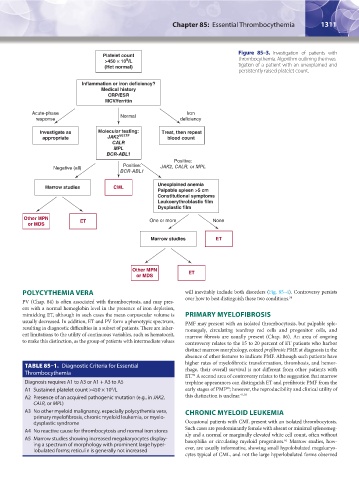
Figure 85–3. Investigation of patients with
Platelet count
9
>450 ë 10 /L thrombocythemia. Algorithm outlining the inves-
(Hct normal) tigation of a patient with an unexplained and
persistently raised platelet count.
Inflammation or iron deficiency?
Medical history
CRP/ESR
MCV/ferritin
Acute-phase Normal Iron
response deficiency
Investigate as Molecular testing: Treat, then repeat
appropriate JAK2 V617F blood count
CALR
MPL
BCR-ABL1
Positive:
Negative (all) Positive: JAK2, CALR, or MPL
BCR-ABL1
Unexplained anemia
Marrow studies CML
Palpable spleen >5 cm
Constitutional symptoms
Leukoerythroblastic film
Dysplastic film
Other MPN One or more None
or MDS ET
Marrow studies ET
Other MPN ET
or MDS
POLYCYTHEMIA VERA will inevitably include both disorders (Fig. 85–4). Controversy persists
over how to best distinguish these two conditions. 58
PV (Chap. 84) is often associated with thrombocytosis, and may pres-
ent with a normal hemoglobin level in the presence of iron depletion,
mimicking ET, although in such cases the mean corpuscular volume is PRIMARY MYELOFIBROSIS
usually decreased. In addition, ET and PV form a phenotypic spectrum, PMF may present with an isolated thrombocytosis, but palpable sple-
resulting in diagnostic difficulties in a subset of patients. There are inher- nomegaly, circulating teardrop red cells and progenitor cells, and
ent limitations to the utility of continuous variables, such as hematocrit, marrow fibrosis are usually present (Chap. 86). An area of ongoing
to make this distinction, as the group of patients with intermediate values controversy relates to the 15 to 20 percent of ET patients who harbor
distinct marrow morphology, coined prefibrotic PMF, at diagnosis in the
absence of other features to indicate PMF. Although such patients have
higher rates of myelofibrotic transformation, thrombosis, and hemor-
TABLE 85–1. Diagnostic Criteria for Essential rhage, their overall survival is not different from other patients with
Thrombocythemia
ET. A second area of controversy relates to the suggestion that marrow
59
Diagnosis requires A1 to A3 or A1 + A3 to A5 trephine appearances can distinguish ET and prefibrotic PMF from the
60
A1 Sustained platelet count >450 × 10 /L early stages of PMF ; however, the reproducibility and clinical utility of
9
A2 Presence of an acquired pathogenic mutation (e.g., in JAK2, this distinction is unclear. 41,58
CALR, or MPL)
A3 No other myeloid malignancy, especially polycythemia vera, CHRONIC MYELOID LEUKEMIA
primary myelofibrosis, chronic myeloid leukemia, or myelo-
dysplastic syndrome Occasional patients with CML present with an isolated thrombocytosis.
A4 No reactive cause for thrombocytosis and normal iron stores Such cases are predominantly female with absent or minimal splenomeg-
A5 Marrow studies showing increased megakaryocytes display- aly and a normal or marginally elevated white cell count, often without
61
basophilia or circulating myeloid progenitors. Marrow studies, how-
ing a spectrum of morphology with prominent large hyper-
lobulated forms; reticulin is generally not increased ever, are usually informative, showing small hypolobulated megakaryo-
cytes typical of CML, and not the large hyperlobulated forms observed
Kaushansky_chapter 85_p1307-1318.indd 1311 9/21/15 11:08 AM