Page 1033 - Clinical Immunology_ Principles and Practice ( PDFDrive )
P. 1033
996 Part seven Organ-Specific Inflammatory Disease
TABLE 74.2 Characteristic Features of
Common Forms of Uveitis
Parameter
Location Anterior: ankylosing spondylitis, reactive arthritis,
juvenile idiopathic arthritis
Intermediate: Pars planitis
Posterior: Vogt-Koyanagi-Harada syndrome (panuveitis
most common)
Onset Sudden: ankylosing spondylitis, reactive arthritis
Insidious: pars planitis, juvenile idiopathic arthritis
Symmetry Unilateral: ankylosing spondylitis, toxoplasmosis,
herpetic
Bilateral: pars planitis, lymphoma, juvenile idiopathic
arthritis
Course Self-limiting: toxoplasmosis
Recurrent: Behçet disease, ankylosing spondylitis
Chronic: pars planitis
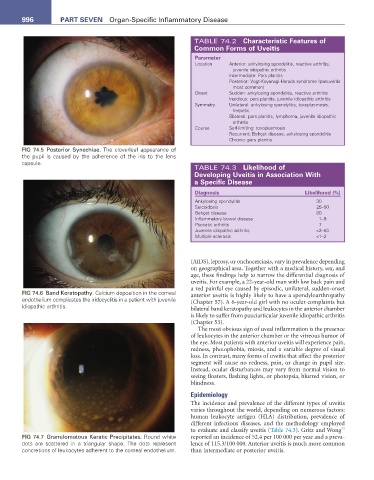
FIG 74.5 Posterior Synechiae. The cloverleaf appearance of
the pupil is caused by the adherence of the iris to the lens
capsule.
TABLE 74.3 Likelihood of
Developing Uveitis in association With
a specific Disease
Diagnosis Likelihood (%)
Ankylosing spondylitis 30
Sarcoidosis 25–50
Behçet disease 80
Inflammatory bowel disease 1–9
Psoriatic arthritis 7
Juvenile idiopathic arthritis <2–53
Multiple sclerosis <1–2
(AIDS), leprosy, or onchocerciasis, vary in prevalence depending
on geographical area. Together with a medical history, sex, and
age, these findings help to narrow the differential diagnosis of
uveitis. For example, a 22-year-old man with low back pain and
a red painful eye caused by episodic, unilateral, sudden-onset
FIG 74.6 Band Keratopathy. Calcium deposition in the corneal anterior uveitis is highly likely to have a spondyloarthropathy
endothelium complicates the iridocyclitis in a patient with juvenile (Chapter 57). A 6-year-old girl with no ocular complaints but
idiopathic arthritis. bilateral band keratopathy and leukocytes in the anterior chamber
is likely to suffer from pauciarticular juvenile idiopathic arthritis
(Chapter 53).
The most obvious sign of uveal inflammation is the presence
of leukocytes in the anterior chamber or the vitreous humor of
the eye. Most patients with anterior uveitis will experience pain,
redness, photophobia, miosis, and a variable degree of visual
loss. In contrast, many forms of uveitis that affect the posterior
segment will cause no redness, pain, or change in pupil size.
Instead, ocular disturbances may vary from normal vision to
seeing floaters, flashing lights, or photopsia, blurred vision, or
blindness.
Epidemiology
The incidence and prevalence of the different types of uveitis
varies throughout the world, depending on numerous factors:
human leukocyte antigen (HLA) distribution, prevalence of
different infectious diseases, and the methodology employed
14
to evaluate and classify uveitis (Table 74.3). Gritz and Wong
FIG 74.7 Granulomatous Keratic Precipitates. Round white reported an incidence of 52.4 per 100 000 per year and a preva-
dots are scattered in a triangular shape. The dots represent lence of 115.3/100 000. Anterior uveitis is much more common
concretions of leukocytes adherent to the corneal endothelium. than intermediate or posterior uveitis.