Page 1036 - Clinical Immunology_ Principles and Practice ( PDFDrive )
P. 1036
CHaPter 74 Immunological Ocular Disease 999
KeY COnCePt TABLE 74.4 systemic Immune-Mediated
Diseases associated With scleritis
Unilateral, recurrent, acute anterior uveitis is one of the most common
forms of uveitis; it is frequently associated with spondyloarthritis. Rheumatoid arthritis
Granulomatosis with polyangiitis
Inflammatory bowel disease
Polyarteritis nodosa
Temporal arteritis/giant cell arteritis
CLInICaL PearL Systemic lupus erythematosus
Ankylosing spondylitis
It is important to rule out infectious causes of uveitis before initiating Relapsing polychondritis
immunosuppression for uveitis.
Advancements and New Treatments for Uveitis
As molecular diagnostics, such as next-generation deep sequencing
techniques and bioinformatics, are becoming refined and more
broadly available, additional etiological agents for uveitis may
be discovered. Additionally, with an increased understanding of
the cellular pathways involved in various uveitic entities, new
targets for therapy of uveitis may emerge. For instance, targeting
IL-6 with a biologic agent versus targeting lymphocyte trafficking
to the eye via an antibody against adhesion molecules may
represent emerging therapies. Additional local drug delivery
methods may improve ocular efficacy while lowering systemic
side effects.
On tHe HOrIZOn
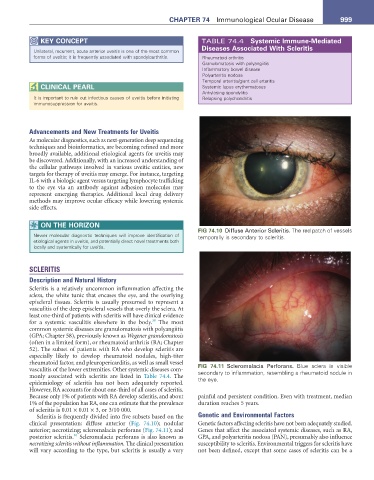
FIG 74.10 Diffuse Anterior Scleritis. The red patch of vessels
Newer molecular diagnostic techniques will improve identification of temporally is secondary to scleritis.
etiological agents in uveitis, and potentially direct novel treatments both
locally and systemically for uveitis.
SCLERITIS
Description and Natural History
Scleritis is a relatively uncommon inflammation affecting the
sclera, the white tunic that encases the eye, and the overlying
episcleral tissues. Scleritis is usually presumed to represent a
vasculitis of the deep episcleral vessels that overly the sclera. At
least one-third of patients with scleritis will have clinical evidence
39
for a systemic vasculitis elsewhere in the body. The most
common systemic diseases are granulomatosis with polyangiitis
(GPA; Chapter 58), previously known as Wegener granulomatosis
(often in a limited form), or rheumatoid arthritis (RA; Chapter
52). The subset of patients with RA who develop scleritis are
especially likely to develop rheumatoid nodules, high-titer
rheumatoid factor, and pleuropericarditis, as well as small vessel FIG 74.11 Scleromalacia Perforans. Blue sclera is visible
vasculitis of the lower extremities. Other systemic diseases com- secondary to inflammation, resembling a rheumatoid nodule in
monly associated with scleritis are listed in Table 74.4. The the eye.
epidemiology of scleritis has not been adequately reported.
However, RA accounts for about one-third of all cases of scleritis.
Because only 1% of patients with RA develop scleritis, and about painful and persistent condition. Even with treatment, median
1% of the population has RA, one can estimate that the prevalence duration reaches 5 years.
of scleritis is 0.01 × 0.01 × 3, or 3/10 000.
Scleritis is frequently divided into five subsets based on the Genetic and Environmental Factors
clinical presentation: diffuse anterior (Fig. 74.10); nodular Genetic factors affecting scleritis have not been adequately studied.
anterior; necrotizing; scleromalacia perforans (Fig. 74.11); and Genes that affect the associated systemic diseases, such as RA,
40
posterior scleritis. Scleromalacia perforans is also known as GPA, and polyarteritis nodosa (PAN), presumably also influence
necrotizing scleritis without inflammation. The clinical presentation susceptibility to scleritis. Environmental triggers for scleritis have
will vary according to the type, but scleritis is usually a very not been defined, except that some cases of scleritis can be a