Page 398 - Clinical Immunology_ Principles and Practice ( PDFDrive )
P. 398
CHAPtER 26 Host Defenses to Intracellular Bacteria 379
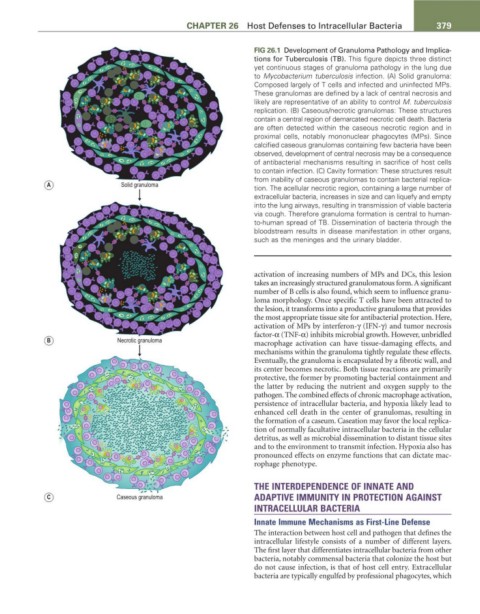
FIG 26.1 Development of Granuloma Pathology and Implica-
tions for Tuberculosis (TB). This figure depicts three distinct
yet continuous stages of granuloma pathology in the lung due
to Mycobacterium tuberculosis infection. (A) Solid granuloma:
Composed largely of T cells and infected and uninfected MPs.
These granulomas are defined by a lack of central necrosis and
likely are representative of an ability to control M. tuberculosis
replication. (B) Caseous/necrotic granulomas: These structures
contain a central region of demarcated necrotic cell death. Bacteria
are often detected within the caseous necrotic region and in
proximal cells, notably mononuclear phagocytes (MPs). Since
calcified caseous granulomas containing few bacteria have been
observed, development of central necrosis may be a consequence
of antibacterial mechanisms resulting in sacrifice of host cells
to contain infection. (C) Cavity formation: These structures result
from inability of caseous granulomas to contain bacterial replica-
A Solid granuloma tion. The acellular necrotic region, containing a large number of
extracellular bacteria, increases in size and can liquefy and empty
into the lung airways, resulting in transmission of viable bacteria
via cough. Therefore granuloma formation is central to human-
to-human spread of TB. Dissemination of bacteria through the
bloodstream results in disease manifestation in other organs,
such as the meninges and the urinary bladder.
activation of increasing numbers of MPs and DCs, this lesion
takes an increasingly structured granulomatous form. A significant
number of B cells is also found, which seem to influence granu-
loma morphology. Once specific T cells have been attracted to
the lesion, it transforms into a productive granuloma that provides
the most appropriate tissue site for antibacterial protection. Here,
activation of MPs by interferon-γ (IFN-γ) and tumor necrosis
factor-α (TNF-α) inhibits microbial growth. However, unbridled
B Necrotic granuloma macrophage activation can have tissue-damaging effects, and
mechanisms within the granuloma tightly regulate these effects.
Eventually, the granuloma is encapsulated by a fibrotic wall, and
its center becomes necrotic. Both tissue reactions are primarily
protective, the former by promoting bacterial containment and
the latter by reducing the nutrient and oxygen supply to the
pathogen. The combined effects of chronic macrophage activation,
persistence of intracellular bacteria, and hypoxia likely lead to
enhanced cell death in the center of granulomas, resulting in
the formation of a caseum. Caseation may favor the local replica-
tion of normally facultative intracellular bacteria in the cellular
detritus, as well as microbial dissemination to distant tissue sites
and to the environment to transmit infection. Hypoxia also has
pronounced effects on enzyme functions that can dictate mac-
rophage phenotype.
THE INTERDEPENDENCE OF INNATE AND
C Caseous granuloma ADAPTIVE IMMUNITY IN PROTECTION AGAINST
INTRACELLULAR BACTERIA
Innate Immune Mechanisms as First-Line Defense
The interaction between host cell and pathogen that defines the
intracellular lifestyle consists of a number of different layers.
The first layer that differentiates intracellular bacteria from other
bacteria, notably commensal bacteria that colonize the host but
do not cause infection, is that of host cell entry. Extracellular
bacteria are typically engulfed by professional phagocytes, which