Page 394 - Clinical Immunology_ Principles and Practice ( PDFDrive )
P. 394
26
Host Defenses to Intracellular Bacteria
Stephen T. Reece, Stefan H.E. Kaufmann
The evolutionary relationship between humans and bacteria is CLINICAL PEARLS
so intimate that it is impossible to imagine the development of
1
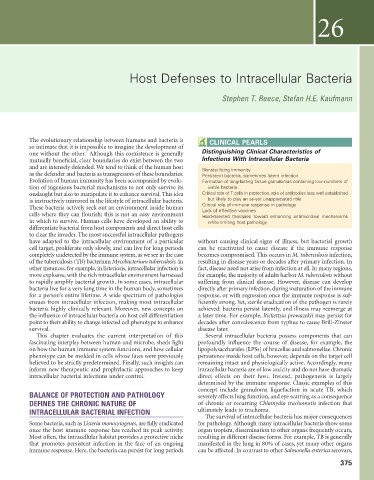
one without the other. Although this coexistence is generally Distinguishing Clinical Characteristics of
mutually beneficial, clear boundaries do exist between the two Infections With Intracellular Bacteria
and are intensely defended. We tend to think of the human host Nonsterilizing immunity
as the defender and bacteria as transgressors of these boundaries. Persistent bacteria, sometimes latent infection
Evolution of human immunity has been accompanied by evolu- Formation of long-lasting tissue granulomas containing low numbers of
tion of ingenious bacterial mechanisms to not only survive its viable bacteria
onslaught but also to manipulate it to enhance survival. This idea Critical role of T cells in protection, role of antibodies less well established
is instructively mirrored in the lifestyle of intracellular bacteria. but likely to play an as-yet unappreciated role
These bacteria actively seek out an environment inside human Critical role of immune response in pathology
Lack of effective vaccines
cells where they can flourish; this is not an easy environment Host-directed therapies toward enhancing antimicrobial mechanisms
in which to survive. Human cells have developed an ability to while limiting host pathology
differentiate bacterial from host components and direct host cells
to clear the invader. The most successful intracellular pathogens
have adapted to the intracellular environment of a particular without causing clinical signs of illness, but bacterial growth
cell target, proliferate only slowly, and can live for long periods can be reactivated to cause disease if the immune response
completely undetected by the immune system, as we see in the case becomes compromised. This occurs in M. tuberculosis infection,
of the tuberculosis (TB) bacterium Mycobacterium tuberculosis. In resulting in disease years or decades after primary infection. In
other instances, for example, in listeriosis, intracellular infection is fact, disease need not arise from infection at all. In many regions,
more explosive, with the rich intracellular environment harnessed for example, the majority of adults harbor M. tuberculosis without
to rapidly amplify bacterial growth. In some cases, intracellular suffering from clinical disease. However, disease can develop
bacteria live for a very long time in the human body, sometimes directly after primary infection, during maturation of the immune
for a person’s entire lifetime. A wide spectrum of pathologies response, or with regression once the immune response is suf-
ensues from intracellular infection, making most intracellular ficiently strong. Yet, sterile eradication of the pathogen is rarely
bacteria highly clinically relevant. Moreover, new concepts on achieved: bacteria persist latently, and illness may reemerge at
the influence of intracellular bacteria on host cell differentiation a later time. For example, Rickettsia prowazekii may persist for
point to their ability to change infected cell phenotype to enhance decades after convalescence from typhus to cause Brill-Zinsser
survival. disease later.
This chapter evaluates the current interpretation of this Several intracellular bacteria possess components that can
fascinating interplay between human and microbe, sheds light profoundly influence the course of disease, for example, the
on how the human immune system functions, and how cellular lipopolysaccharides (LPSs) of brucellae and salmonellae. Chronic
phenotype can be molded in cells whose fates were previously persistence inside host cells, however, depends on the target cell
believed to be strictly predetermined. Finally, such insights can remaining intact and physiologically active. Accordingly, many
inform new therapeutic and prophylactic approaches to keep intracellular bacteria are of low toxicity and do not have dramatic
intracellular bacterial infections under control. direct effects on their host. Instead, pathogenesis is largely
determined by the immune response. Classic examples of this
concept include granuloma liquefaction in acute TB, which
BALANCE OF PROTECTION AND PATHOLOGY severely affects lung function, and eye scarring as a consequence
DEFINES THE CHRONIC NATURE OF of chronic or recurring Chlamydia trachomatis infection that
INTRACELLULAR BACTERIAL INFECTION ultimately leads to trachoma.
The survival of intracellular bacteria has major consequences
Some bacteria, such as Listeria monocytogenes, are fully eradicated for pathology. Although many intracellular bacteria show some
once the host immune response has reached its peak activity. organ tropism, dissemination to other organs frequently occurs,
Most often, the intracellular habitat provides a protective niche resulting in different disease forms. For example, TB is generally
that promotes persistent infection in the face of an ongoing manifested in the lung in 80% of cases, yet many other organs
immune response. Here, the bacteria can persist for long periods can be affected. In contrast to other Salmonella enterica serovars,
375