Page 1177 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 1177
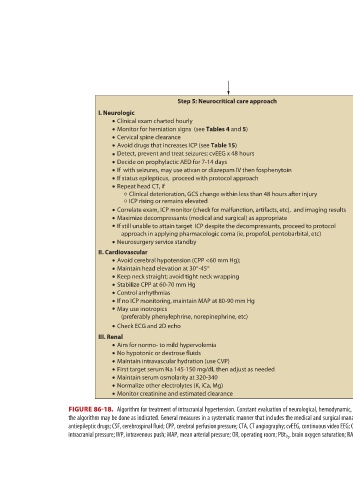
antiepileptic drugs; CSF, cerebrospinal fluid; CPP, cerebral perfusion pressure; CTA, CT angiography; cvEEG, continuous video EEG; CVP, central venous pressure; DVT, deep vein thrombosis; EVD, external ventricular drainage; GCS, Glasgow Coma Scale; ICP,
ICP; <20 mm Hg; CPP; 60-70 mm Hg, CVP; 10-12 mm Hg; Pa O 2 ; >80 mm Hg;
If heparin or LMWH is considered, caution if existing coagulopathy
Normalize bleeding parameters (eg, platelet count >100 k/mL)
Minimize noxious stimuli upon examination and bedside care
Maintain glucose 140-180 mg/dL; avoid hypoglycemia
Brain temp; <37°C; PBt O 2 ; >20 mm Hg
Summary of brain target goals
Analgesia, eg, morphine IV or fentanyl infusion
Sedation, eg, propofol drip titrate to RASS-2
Aim for normothermia (Brain temp <37°C)
Examine patient off sedation, if ICP stable
Paralytics if indicted, eg, vecuronium
If febrile and with EVD, examine CSF
Prokinetic medications, if with ileus
DVT prophylaxis within 24-72 hours
Prevent shivering
VI. Infectious Disease
VIII. Endocrinology
VII. Hematology
IV. Pulmonary
IX. Pain
If still unable to attain target ICP despite the decompressants, proceed to protocol
approach in applying pharmacologic coma (ie, propofol, pentobarbital, etc)
Maximize decompressants (medical and surgical) as appropriate
Step 5: Neurocritical care approach Protect and secure airways Spine precautions in trauma patients Avoid hypoxia; goal Pa O 2 >80 mm Hg Goal O 2 sat >90% Keep Pa CO 2 35-38 mm Hg No prolonged hyperventilation Hyperventilation may be used for ICP crises or pending herniation Avoid hypercapnia (vasoconstriction may produce ischemia) Do ABGs and use end tidal CO 2 Do chest x-ray If with seizures, may use ativan or diazepam IV then fosphenytoin V. Gastroenterology Early feeding (within 24 hours) Clinical deterioration, GCS change within less than 48 hours after injury Maximize caloric feeding for crit
First target serum Na 145-150 mg/dL then adjust as needed
Clinical exam charted hourly Monitor for herniation signs (see Tables 4 and 5) Cervical spine clearance Avoid drugs that increases ICP (see Table 15) Detect, prevent and treat seizures; cvEEG x 48 hours Decide on prophylactic AED for 7-14 days If status epilepticus, proceed with protocol approach Repeat head CT, if ICP rising or remains elevated Neurosurgery service standby Avoid cerebral hypotension (CPP <60 mm Hg); Maintain head elevation at 30°-45° Keep neck straight; avoid tight neck wrapping Stabilize CPP at 60-70 mm Hg Control arrhythmias If no ICP monitoring, maintain MAP at 80-90 mm Hg
I. Neurologic II. Cardiovascular III. Renal
FIGURE 86-18.
section06.indd 815 1/23/2015 12:56:11 PM