Page 1172 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 1172
CHAPTER 86: Intracranial Pressure: Monitoring and Management 811
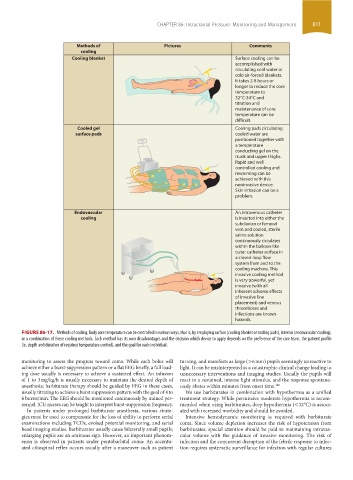
Methods of Pictures Comments
cooling
Cooling blanket Surface cooling can be
accomplished with
circulating cold water or
cold air-forced blankets.
It takes 2-8 hours or
longer to reduce the core
temperature to
32°C-34°C and
titration and
maintenance of core
temperature can be
difficult.
Cooled gel Cooling pads circulating
surface pads cooled water are
positioned together with
a temperature
conducting gel on the
trunk and upper thighs.
Rapid and well
controlled cooling and
rewarming can be
achieved with this
noninvasive device.
Skin irritation can be a
problem.
Endovascular An intravenous catheter
cooling is inserted into either the
subclavian or femoral
vein and cooled, sterile
saline solution
continuously circulates
within the balloon-like
outer catheter surface in
a closed-loop flow
system from and to the
cooling machine. This
invasive cooling method
is very powerful, yet
invasive (with all
inherent adverse effects
of invasive line
placement) and venous
thromboses and
infections are known
hazards.
FIGURE 86-17. Methods of cooling. Body core temperature can be controlled in various ways, that is, by employing surface (cooling blanket or cooling pads), internal (endovascular cooling),
or a combination of these cooling methods. Each method has its own disadvantages and the decision which device to apply depends on the preference of the care team, the patient profile
(ie, depth and duration of required temperature control), and the goal for each individual.
monitoring to assess the progress toward coma. While each bolus will turning, and manifests as large (>6 mm) pupils seemingly unreactive to
achieve either a burst-suppression pattern or a flat EEG briefly, a full load- light. It can be misinterpreted as a catastrophic clinical change leading to
ing dose usually is necessary to achieve a sustained effect. An infusion unnecessary interventions and imaging studies. Usually the pupils will
of 1 to 3 mg/kg/h is usually necessary to maintain the desired depth of react to a sustained, intense light stimulus, and the response spontane-
anesthesia; barbiturate therapy should be guided by EEG in these cases, ously abates within minutes from onset time. 140
usually titrating to achieve a burst suppression pattern with the goal of 4 to We use barbiturates in combination with hypothermia as a unified
6 bursts/min. The EEG should be monitored continuously by trained per- treatment strategy. While permissive moderate hypothermia is recom-
sonnel. ICU nurses can be taught to interpret burst-suppression frequency. mended when using barbiturates, deep hypothermia (<32°C) is associ-
In patients under prolonged barbiturate anesthesia, various strate- ated with increased morbidity and should be avoided.
gies must be used to compensate for the loss of ability to perform serial Intensive hemodynamic monitoring is required with barbiturate
examinations including TCDs, evoked potential monitoring, and serial coma. Since volume depletion increases the risk of hypotension from
head imaging studies. Barbiturates usually cause bilaterally small pupils; barbiturates, special attention should be paid to maintaining intravas-
enlarging pupils are an ominous sign. However, an important phenom- cular volume with the guidance of invasive monitoring. The risk of
enon is observed in patients under pentobarbital coma: An accentu- infection and the concurrent disruption of the febrile response to infec-
ated ciliospinal reflex occurs usually after a maneuver such as patient tion requires systematic surveillance for infection with regular cultures
section06.indd 811 1/23/2015 12:56:08 PM