Page 1347 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 1347
920 PART 8: Renal and Metabolic Disorders
Tubular damage
Ischemia
nephrotoxins (proximal tubules and
ascending thick limb
(1) (2) (3) (4)
Vasoconstriction Obstruction Tubular Interstitial
renin-angiotensin by casts backleak inflammation
endothelin
PGI 2
https://kat.cr/user/tahir99/
NO
Intratubular Tubular
pressure fluid flow
(5)
? Direct glomerular GFR Oliguria
effect
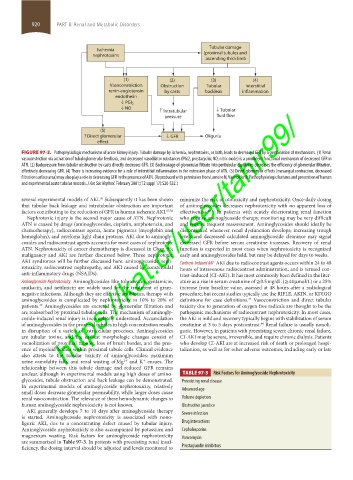
FIGURE 97-2. Pathophysiologic mechanisms of acute kidney injury. Tubular damage by ischemia, nephrotoxins, or both, leads to decreased GFR by a combination of mechanisms. (1) Renal
vasoconstriction via activation of tubuloglomerular feedback, and decreased vasodilator substances (PGI2, prostacyclin; NO, nitric oxide) is a prominent functional mechanism of decreased GFR in
ATN. (2) Backpressure from tubular obstruction by casts directly decreases GFR. (3) Backleakage of glomerular filtrate into peritubular capillaries decreases the efficiency of glomerular filtration,
effectively decreasing GFR. (4) There is increasing evidence for a role of interstitial inflammation in the extension phase of ATN. (5) Direct glomerular effects (mesangial contraction, decreased
filtration surface area) may also play a role in decreasing GFR in the presence of ATN. (Reproduced with permission from Lameire N, Vanholder R. Pathophysiologic features and prevention of human
and experimental acute tubular necrosis. J Am Soc Nephrol. February 2001;(12 suppl 17):S20-S32.)
several experimental models of AKI. Subsequently it has been shown minimize the risk of ototoxicity and nephrotoxicity. Once-daily dosing
36
that tubular back leakage and intratubular obstruction are important of aminoglycosides decreases nephrotoxicity with no apparent loss of
factors contributing to the reduction of GFR in human ischemic AKI. 37,38 effectiveness. 40-42 In patients with acutely deteriorating renal function
Nephrotoxic injury is the second major cause of ATN. Nephrotoxic who require aminoglycoside therapy, monitoring may be very difficult
ATN is caused by drugs (aminoglycosides, cisplatin, amphotericin, and and require frequent reassessment. Aminoglycosides should ideally be
chemotherapy), radiocontrast agents, heme pigments (myoglobin and discontinued whenever renal dysfunction develops; increasing trough
hemoglobin), and myeloma light chain proteins. AKI due to aminogly- levels and decreased calculated aminoglycoside clearance may signal
cosides and radiocontrast agents accounts for most cases of nephrotoxic decreased GFR before serum creatinine increases. Recovery of renal
ATN. Nephrotoxicity of cancer chemotherapy is discussed in Chap. 95; function is expected in most cases when nephrotoxicity is recognized
malignancy and AKI are further discussed below. Three nephrotoxic early and aminoglycosides held, but may be delayed for days to weeks.
AKI syndromes will be further discussed here: aminoglycoside neph- Contrast-Induced AKI AKI due to radiocontrast agents occurs within 24 to 48
rotoxicity, radiocontrast nephropathy, and AKI caused by nonsteroidal hours of intravenous radiocontrast administration, and is termed con-
anti-inflammatory drugs (NSAIDs). trast-induced (CI-AKI). It has most commonly been defined in the liter-
Aminoglycoside Nephrotoxicity Aminoglycosides like tobramycin, gentamicin, ature as a rise in serum creatinine of ≥0.5 mg/dL (≥44 µmol/L) or a 25%
amikacin, and netilmicin are widely used for the treatment of gram- increase from baseline value, assessed at 48 hours after a radiological
negative infections. Although they are effective antibiotics, therapy with procedure; but recent studies typically use the RIFLE, AKIN, or KDIGO
aminoglycosides is complicated by nephrotoxicity in 10% to 20% of definitions for case definitions. Vasoconstriction and direct tubular
43
patients. Aminoglycosides are excreted by glomerular filtration and toxicity due to generation of oxygen free radicals are thought to be the
39
are reabsorbed by proximal tubular cells. The mechanism of aminogly- pathogenic mechanisms of radiocontrast nephrotoxicity. In most cases,
coside-induced renal injury is incompletely understood. Accumulation the AKI is mild and recovery typically begins with stabilization of serum
of aminoglycosides in the proximal tubules in high concentration results creatinine at 3 to 5 days postcontrast. Renal failure is usually nonoli-
44
in disruption of a variety of intracellular processes. Aminoglycosides guric. However, in patients with preexisting severe chronic renal failure,
are tubular toxins, and the earliest morphologic changes consist of CI-AKI may be severe, irreversible, and require chronic dialysis. Patients
vacuolization of proximal tubules, loss of brush border, and the pres- who develop CI-AKI are at increased risk of death or prolonged hospi-
ence of myeloid bodies within proximal tubule cells. Clinical evidence talization, as well as for other adverse outcomes, including early or late
also attests to the tubular toxicity of aminoglycosides; maximum
urine osmolality falls, and renal wasting of Mg and K ensues. The
+
2+
relationship between this tubule damage and reduced GFR remains
unclear, although in experimental models using high doses of amino- TABLE 97-3 Risk Factors for Aminoglycoside Nephrotoxicity
glycosides, tubule obstruction and back leakage can be demonstrated. Preexisting renal disease
In experimental models of aminoglycoside nephrotoxicity, relatively Advanced age
small doses decrease glomerular permeability, while larger doses cause
renal vasoconstriction. The relevance of these hemodynamic changes to Volume depletion
human aminoglycoside nephrotoxicity is not known. Obstructive jaundice
AKI generally develops 7 to 10 days after aminoglycoside therapy
is started. Aminoglycoside nephrotoxicity is associated with nono- Severe infection
liguric AKI, due to a concentrating defect caused by tubular injury. Drug interactions
Aminoglycoside nephrotoxicity is also accompanied by potassium and Cephalosporins
magnesium wasting. Risk factors for aminoglycoside nephrotoxicity Vancomycin
are summarized in Table 97-3. In patients with preexisting renal insuf-
ficiency, the dosing interval should be adjusted and levels monitored to Prostaglandin inhibitors
section08.indd 920 1/14/2015 8:27:53 AM