Page 1572 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 1572
CHAPTER 115: The Transplant Patient 1091
3000
CF Alfa-1
IPF IPAH
2500
COPD Re-Tx
Number of transplants 1500
2000
1000
500
0
1990 1991 1992 1993 1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011
Transplant year
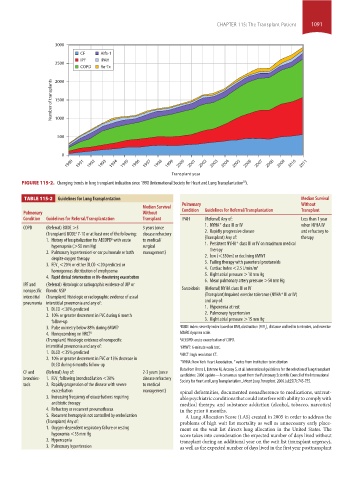
FIGURE 115-2. Changing trends in lung transplant indication since 1990 (International Society for Heart and Lung Transplantation ).
30
TABLE 115-2 Guidelines for Lung Transplantation
TABLE 115-2 Guidelines for Lung Transplantation Median Survival
Pulmonary Without
Median Survival
Pulmonary Without Condition Guidelines for Referral/Transplantation Transplant
Condition Guidelines for Referral/Transplantation Transplant IPAH (Referral) Any of: Less than 1 year
+
1. NYHA class III or IV when NYHA IV
COPD (Referral) BODE >5 3 years (once
(Transplant) BODE 7-10 or at least one of the following: disease refractory 2. Rapidly progressive disease and refractory to
a
1. History of hospitalization for AECOPD with acute to medical/ (Transplant) Any of: + therapy
b
hypercapnia (>50 mm Hg) surgical 1. Persistent NYHA class III or IV on maximum medical
c
2. Pulmonary hypertension or cor pulmonale or both management) therapy
despite oxygen therapy 2. low (<350 m) or declining 6MWT
3. FEV <20% or either DLCO <20 predicted or 3. Failing therapy with parenteral prostanoids
2
1
homogenous distribution of emphysema 4. Cardiac Index <2.5 L/min/m
4. Rapid clinical deterioration or life-threatening exacerbation 5. Right atrial pressure >10 mm Hg
6. Mean pulmonary artery pressure >50 mm Hg
IPF and (Referral) Histologic or radiographic evidence of UIP or
nonspecific fibrotic NSIP Sarcoidosis (Referral) NYHA class III or IV +
interstitial (Transplant) Histologic or radiographic evidence of usual (Transplant)Impaired exercise tolerance (NYHA III or IV)
pneumonia interstitial pneumonia and any of: and any of:
1. DLCO <30% predicted 1. Hypoxemia at rest
2. 10% or greater decrement in FVC during 6 month 2. Pulmonary hypertension
follow-up 3. Right atrial pressure >15 mm Hg
3. Pulse oximetry below 88% during 6MWT c a BODE index: severity index based on BMI, obstruction (FEV ), distance walked in 6 minutes, and exercise
1
4. Honeycombing on HRCT d MMRC dyspnea scale.
(Transplant) Histologic evidence of nonspecific b AECOPD: acute exacerbation of COPD.
interstitial pneumonia and any of: c 6MWT: 6-minute walk test.
1. DLCO <35% predicted d HRCT: high resolution CT.
2. 10% or greater decrement in FVC or 15% decrease in + +
DLCO during 6 months follow-up NYHA: New York Heart Association. varies from institution to institution
Data from Orens J, Estenne M, Arcasoy S, et al. International guidelines for the selection of lung transplant
CF and (Referral) Any of: 2-3 years (once
bronchiec- 1. FEV following bronchodilation <30% disease refractory candidates: 2006 update—A consensus report from the Pulmonary Scientific Council of the International
Society for Heart and Lung Transplantation. J Heart Lung Transplant. 2006 Jul;25(7):745-755.
1
tasis 2. Rapidly progression of the disease with severe to medical
exacerbation management) spinal deformities, documented nonadherence to medications, untreat-
3. Increasing frequency of exacerbations requiring able psychiatric conditions that could interfere with ability to comply with
antibiotic therapy medical therapy, and substance addiction (alcohol, tobacco, narcotics)
4. Refractory or recurrent pneumothorax in the prior 6 months.
5. Recurrent hemoptysis not controlled by embolization A Lung Allocation Score (LAS) created in 2005 in order to address the
(Transplant) Any of: problems of high wait list mortality as well as unnecessary early place-
1. Oxygen-dependent respiratory failure or resting ment on the wait list directs lung allocation in the United States. The
hypoxemia <55 mm Hg score takes into consideration the expected number of days lived without
2. Hypercapnia transplant during an additional year on the wait list (transplant urgency),
3. Pulmonary hypertension as well as the expected number of days lived in the first year posttransplant
section10.indd 1091 1/20/2015 9:19:53 AM