Page 1831 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 1831
1300 PART 11: Special Problems in Critical Care
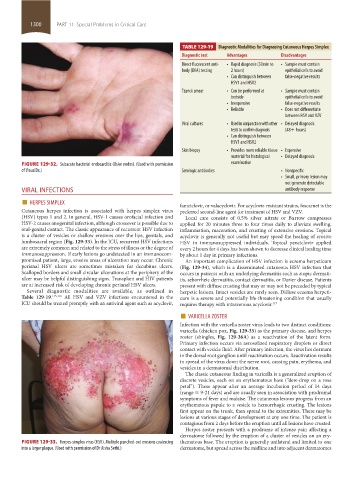
TABLE 129-19 Diagnostic Modalities for Diagnosing Cutaneous Herpes Simplex
Diagnostic test Advantages Disadvantages
Direct fluorescent anti- • Rapid diagnosis (30min to • Sample must contain
body (DFA) testing 2 hours) epithelial cells to avoid
• Can distinguish between false-negative results
HSV1 and HSV2
Tzanck smear • Can be performed at • Sample must contain
bedside epithelial cells to avoid
• Inexpensive false-negative results
• Reliable • Does not differentiate
between HSV and VZV
Viral cultures • Used in conjunction with other • Delayed diagnosis
tests to confirm diagnosis (48+ hours)
• Can distinguish between
HSV1 and HSV2
Skin biopsy • Provides more reliable tissue • Expensive
material for histological • Delayed diagnosis
FIGURE 129-32. Subacute bacterial endocarditis (Osler nodes). (Used with permission examination
of VisualDx.) Serologic antibodies • Nonspecific
• Small, primary lesion may
not generate detectable
VIRAL INFECTIONS antibody response
■ HERPES SIMPLEX
Cutaneous herpes infection is associated with herpes simplex virus famciclovir, or valacyclovir. For acyclovir-resistant strains, foscarnet is the
preferred second-line agent for treatment of HSV and VZV.
(HSV) types 1 and 2. In general, HSV-1 causes orofacial infection and Local care consists of 0.5% silver nitrate or Burrow compresses
HSV-2 causes anogenital infection, although crossover is possible due to applied for 20 minutes three to four times daily to alleviate swelling,
oral-genital contact. The classic appearance of recurrent HSV infection inflammation, maceration, and crusting of extensive erosions. Topical
is a cluster of vesicles or shallow erosions over the lips, genitals, and acyclovir is generally not useful but may speed the healing of erosive
lumbosacral region (Fig. 129-33). In the ICU, recurrent HSV infections HSV in immunosuppressed individuals. Topical penciclovir applied
are extremely common and related to the stress of illness or the degree of every 2 hours for 4 days has been shown to decrease clinical healing time
immunosuppression. If early lesions go undetected in an immunocom- by about 1 day in primary infections.
promised patient, large, erosive areas of ulceration may occur. Chronic An important complication of HSV infection is eczema herpeticum
perianal HSV ulcers are sometimes mistaken for decubitus ulcers. (Fig. 129-34), which is a disseminated cutaneous HSV infection that
Scalloped borders and small circular ulcerations at the periphery of the occurs in patients with an underlying dermatitis such as atopic dermati-
ulcer may be helpful distinguishing signs. Transplant and HIV patients tis, seborrheic dermatitis, contact dermatitis, or Darier disease. Patients
are at increased risk of developing chronic perianal HSV ulcers. present with diffuse crusting that may or may not be preceded by typical
Several diagnostic modalities are available, as outlined in herpetic lesions. Intact vesicles are rarely seen. Diffuse eczema herpeti-
Table 129-19. 115,116 All HSV and VZV infections encountered in the cum is a severe and potentially life-threatening condition that usually
ICU should be treated promptly with an antiviral agent such as acyclovir, requires therapy with intravenous acyclovir. 117
■ VARICELLA ZOSTER
Infection with the varicella zoster virus leads to two distinct conditions:
varicella (chicken pox, Fig. 129-35) as the primary disease, and herpes
zoster (shingles, Fig. 129-36A) as a reactivation of the latent form.
Primary infection occurs via aerosolized respiratory droplets or direct
contact with vesicle fluid. After primary infection, the virus lies dormant
in the dorsal root ganglion until reactivation occurs. Reactivation results
in spread of the virus down the nerve root, causing pain, erythema, and
vesicles in a dermatomal distribution.
The classic cutaneous finding in varicella is a generalized eruption of
discrete vesicles, each on an erythematous base (“dew-drop on a rose
petal”). These appear after an average incubation period of 14 days
(range = 9-21 days) and are usually seen in association with prodromal
symptoms of fever and malaise. The cutaneous lesions progress from an
erythematous papule to a vesicle to hemorrhagic crusting. The lesions
first appear on the trunk, then spread to the extremities. There may be
lesions at various stages of development at any one time. The patient is
contagious from 2 days before the eruption until all lesions have crusted.
Herpes zoster presents with a prodrome of intense pain affecting a
dermatome followed by the eruption of a cluster of vesicles on an ery-
FIGURE 129-33. Herpes-simplex virus (HSV). Multiple punched-out erosions coalescing thematous base. The eruption is generally unilateral and limited to one
into a larger plaque. (Used with permission of Dr Aisha Sethi.) dermatome, but spread across the midline and into adjacent dermatomes
section11.indd 1300 1/19/2015 10:55:41 AM