Page 1846 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 1846
CHAPTER 131: Hypothermia 1315
Vital signs
Core body temperature
Maintain adequate airway
Continuous ECG monitoring
Warm, humidified oxygen 40-45°C [104-113°F]
Normal saline warmed to 40-42°C [104-107.6°F]
Naloxone, thiamine, D50W
Pulse and perfusing rhythm present?
Yes No
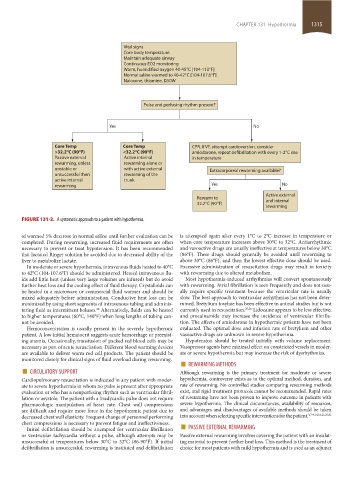
Core Temp Core Temp CPR, If VF, attempt cardioversion, consider
>32.2°C (90°F) <32.2°C (90°F) amiodarone, repeat defibrillation with every 1-2°C rise
Passive external Active internal in temperature
rewarming, unless rewarming alone or
unstable or with active external Extracorporeal rewarming available?
unsuccessful then rewarming of the
active internal trunk
rewarming Yes No
Active external
Rewarm to
32.2°C (90°F) and internal
rewarming
FIGURE 131-2. A systematic approach to a patient with hypothermia.
of warmed 5% dextrose in normal saline until further evaluation can be is attempted again after every 1°C to 2°C increase in temperature or
completed. During rewarming, increased fluid requirements are often when core temperature increases above 30°C to 32°C. Antiarrhythmic
necessary to prevent or treat hypotension. It has been recommended and vasoactive drugs are usually ineffective at temperatures below 30°C
that lactated Ringer solution be avoided due to decreased ability of the (86°F). These drugs should generally be avoided until rewarming to
liver to metabolize lactate. above 30°C (86°F), and then the lowest effective dose should be used.
In moderate or severe hypothermia, intravenous fluids heated to 40°C Excessive administration of resuscitation drugs may result in toxicity
to 42°C (104-107.6°F) should be administered. Heated intravenous flu- with rewarming due to altered metabolism.
ids add little heat (unless very large volumes are infused) but do avoid Most hypothermia-induced arrhythmias will convert spontaneously
further heat loss and the cooling effect of fluid therapy. Crystalloids can with rewarming. Atrial fibrillation is seen frequently and does not usu-
be heated in a microwave or commercial fluid warmer and should be ally require specific treatment because the ventricular rate is usually
mixed adequately before administration. Conductive heat loss can be slow. The best approach to ventricular arrhythmias has not been deter-
minimized by using short segments of intravenous tubing and adminis- mined. Bretylium tosylate has been effective in animal studies but is not
tering fluid as intermittent boluses. Alternatively, fluids can be heated currently used in resuscitation. 27,28 Lidocaine appears to be less effective,
28
to higher temperatures (60°C, 140°F) when long lengths of tubing can- and procainamide may increase the incidence of ventricular fibrilla-
not be avoided. tion. The effects of amiodarone in hypothermic patients have not been
Hemoconcentration is usually present in the severely hypothermic evaluated. The optimal dose and infusion rate of bretylium and other
patient. A low initial hematocrit suggests acute hemorrhage or preexist- vasoactive drugs are unknown in severe hypothermia.
ing anemia. Occasionally, transfusion of packed red blood cells may be Hypotension should be treated initially with volume replacement.
necessary as part of acute resuscitation. Different blood warming devices Vasopressor agents have minimal effect on constricted vessels in moder-
are available to deliver warm red cell products. The patient should be ate or severe hypothermia but may increase the risk of dysrhythmias.
monitored closely for clinical signs of fluid overload during rewarming. ■
■ CIRCULATORY SUPPORT Although rewarming is the primary treatment for moderate or severe
REWARMING METHODS
Cardiopulmonary resuscitation is indicated in any patient with moder- hypothermia, controversy exists as to the optimal method, duration, and
ate to severe hypothermia in whom no pulse is present after appropriate rate of rewarming. No controlled studies comparing rewarming methods
evaluation or who has a nonperfusing rhythm such as ventricular fibril- exist, and rigid treatment protocols cannot be recommended. Rapid rates
lation or asystole. The patient with a bradycardic pulse does not require of rewarming have not been proven to improve outcome in patients with
pharmacologic manipulation of heart rate. Chest wall compressions severe hypothermia. The clinical circumstances, availability of resources,
are difficult and require more force in the hypothermic patient due to and advantages and disadvantages of available methods should be taken
decreased chest wall elasticity. Frequent change of personnel performing into account when selecting specific interventions for the patient. 3,7-9,14,18,21,25,31
Initial defibrillation should be attempted for ventricular fibrillation ■
chest compressions is necessary to prevent fatigue and ineffectiveness. PASSIVE EXTERNAL REWARMING
or ventricular tachycardia without a pulse, although attempts may be Passive external rewarming involves covering the patient with an insulat-
unsuccessful at temperatures below 30°C to 32°C (86-90°F). If initial ing material to prevent further heat loss. This method is the treatment of
defibrillation is unsuccessful, rewarming is instituted and defibrillation choice for most patients with mild hypothermia and is used as an adjunct
section11.indd 1315 1/19/2015 10:56:07 AM