Page 467 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 467
CHAPTER 40: Pericardial Disease 337
tion: Floor:
I aVR V1 V4
II aVL V2 V5
III aVF V3 V6
II
V1
V5
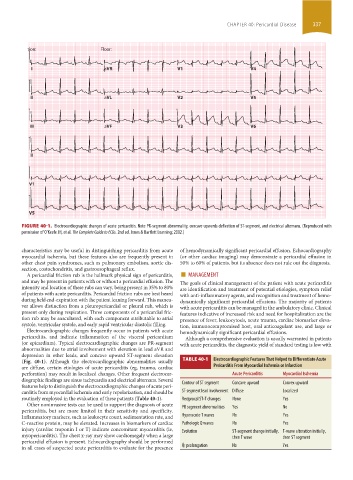
FIGURE 40-1. Electrocardiographic changes of acute pericarditis. Note PR-segment abnormality, concave upwards deflection of ST-segment, and electrical alternans. (Reproduced with
permission of O’Keefe JH, et al. The Complete Guide to ECGs. 2nd ed. Jones & Bartlett Learning; 2002.)
characteristics may be useful in distinguishing pericarditis from acute of hemodynamically significant pericardial effusion. Echocardiography
myocardial ischemia, but these features also are frequently present in (or other cardiac imaging) may demonstrate a pericardial effusion in
other chest pain syndromes, such as pulmonary embolism, aortic dis- 50% to 60% of patients, but its absence does not rule out the diagnosis.
section, costochondritis, and gastroesophageal reflux.
A pericardial friction rub is the hallmark physical sign of pericarditis, ■ MANAGEMENT
and may be present in patients with or without a pericardial effusion. The The goals of clinical management of the patient with acute pericarditis
intensity and location of these rubs can vary, being present in 35% to 80% are identification and treatment of potential etiologies, symptom relief
of patients with acute pericarditis. Pericardial friction rubs are best heard with anti-inflammatory agents, and recognition and treatment of hemo-
during held end-expiration with the patient leaning forward. This maneu- dynamically significant pericardial effusions. The majority of patients
ver allows distinction from a pleuropericardial or pleural rub, which is with acute pericarditis can be managed in the ambulatory clinic. Clinical
present only during respiration. Three components of a pericardial fric- features indicative of increased risk and need for hospitalization are the
tion rub may be auscultated, with each component attributable to atrial presence of fever, leukocytosis, acute trauma, cardiac biomarker eleva-
systole, ventricular systole, and early rapid ventricular diastolic filling. tion, immunocompromised host, oral anticoagulant use, and large or
Electrocardiographic changes frequently occur in patients with acute hemodynamically significant pericardial effusions.
pericarditis, and indicate inflammation of the visceral pericardium Although a comprehensive evaluation is usually warranted in patients
(or epicardium). Typical electrocardiographic changes are PR-segment with acute pericarditis, the diagnostic yield of standard testing is low with
abnormalities due to atrial involvement with elevation in lead aVR and
depression in other leads, and concave upward ST-segment elevation
(Fig. 40-1). Although the electrocardiographic abnormalities usually TABLE 40-1 Electrocardiographic Features That Helped to Differentiate Acute
are diffuse, certain etiologies of acute pericarditis (eg, trauma, cardiac Pericarditis From Myocardial Ischemia or Infarction
perforation) may result in localized changes. Other frequent electrocar- Acute Pericarditis Myocardial Ischemia
diographic findings are sinus tachycardia and electrical alternans. Several
features help to distinguish the electrocardiographic changes of acute peri- Contour of ST segment Concave upward Convex upward
carditis from myocardial ischemia and early repolarization, and should be ST-segment lead involvement Diffuse Localized
routinely employed in the evaluation of these patients (Table 40-1). Reciprocal ST-T changes None Yes
Other noninvasive tests can be used to support the diagnosis of acute PR segment abnormalities Yes No
pericarditis, but are more limited in their sensitivity and specificity.
Inflammatory markers, such as leukocyte count, sedimentation rate, and Hyperacute T waves No Yes
C-reactive protein, may be elevated. Increases in biomarkers of cardiac Pathologic Q waves No Yes
injury (cardiac troponin I or T) indicate concomitant myocarditis (ie, Evolution ST-segment change initially, T-wave alteration initially,
myopericarditis). The chest x-ray may show cardiomegaly when a large then T wave then ST segment
pericardial effusion is present. Echocardiography should be performed
˙
in all cases of suspected acute pericarditis to evaluate for the presence Qt prolongation No Yes
section03.indd 337 1/23/2015 2:07:41 PM