Page 297 - Cardiac Nursing
P. 297
M
Pa
M
8 P
8 P
g
g
g
Pa
Pa
1:1
/09
/09
/29
6
/29
1
1:1
1
/09
1
a
a
a
ara
ara
c.
c.
In
a
In
t
73
A
73
e 2
e 2
p
t
p
A
p
6
26
26
7-2
LWB
LWBK340-c12_
0-c
12_
p
K34
LWB K34 0-c 12_ p pp267-276.qxd 6/29/09 11:18 PM Page 273 Aptara Inc.
q
q
xd
xd
q
76.
7-2
76.
C HAPTER 12 / Radiologic Examination of the Chest 273
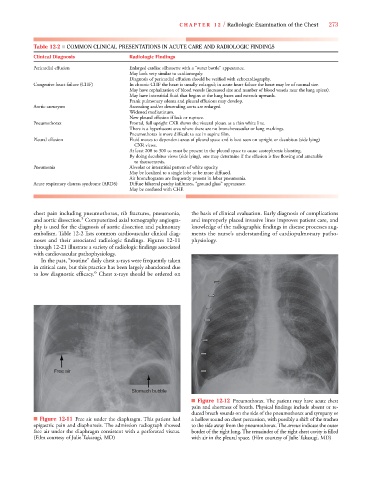
Table 12-2 ■ COMMON CLINICAL PRESENTATIONS IN ACUTE CARE AND RADIOLOGIC FINDINGS
Clinical Diagnosis Radiologic Findings
Pericardial effusion Enlarged cardiac silhouette with a “water bottle” appearance.
May look very similar to cardiomegaly.
Diagnosis of pericardial effusion should be verified with echocardiography.
Congestive heart failure (CHF) In chronic CHF the heart is usually enlarged; in acute heart failure the heart may be of normal size.
May have cephalization of blood vessels (increased size and number of blood vessels near the lung apices).
May have interstitial fluid that begins at the lung bases and extends upwards.
Frank pulmonary edema and pleural effusions may develop.
Aortic aneurysm Ascending and/or descending aorta are enlarged.
Widened mediastinum.
New pleural effusion if leak or rupture.
Pneumothorax Frontal, full upright CXR shows the visceral pleura as a thin white line.
There is a hyperlucent area where there are no bronchovascular or lung markings.
Pneumothorax is more difficult to see in supine film.
Pleural effusion Fluid moves to dependent areas of pleural space and is best seen on upright or decubitus (side lying)
CXR views.
At least 200 to 300 cc must be present in the pleural space to cause costophrenic blunting.
By doing decubitus views (side lying), one may determine if the effusion is free flowing and amenable
to thoracentesis.
Pneumonia Alveolar or interstitial pattern of white opacity.
May be localized to a single lobe or be more diffused.
Air bronchograms are frequently present in lobar pneumonia.
Acute respiratory distress syndrome (ARDS) Diffuse bilateral patchy infiltrates, “ground glass” appearance.
May be confused with CHF.
chest pain including pneumothorax, rib fractures, pneumonia, the basis of clinical evaluation. Early diagnosis of complications
5
and aortic dissection. Computerized axial tomography angiogra- and improperly placed invasive lines improves patient care, and
phy is used for the diagnosis of aortic dissection and pulmonary knowledge of the radiographic findings in disease processes aug-
embolism. Table 12-2 lists common cardiovascular clinical diag- ments the nurse’s understanding of cardiopulmonary patho-
noses and their associated radiologic findings. Figures 12-11 physiology.
through 12-21 illustrate a variety of radiologic findings associated
with cardiovascular pathophysiology.
In the past, “routine” daily chest x-rays were frequently taken
in critical care, but this practice has been largely abandoned due
6
to low diagnostic efficacy. Chest x-rays should be ordered on
Free air
Stomach bubble
■ Figure 12-12 Pneumothorax. The patient may have acute chest
pain and shortness of breath. Physical findings include absent or re-
duced breath sounds on the side of the pneumothorax and tympany or
■ Figure 12-11 Free air under the diaphragm. This patient had a hollow sound on chest percussion, with possibly a shift of the trachea
epigastric pain and diaphoresis. The admission radiograph showed to the side away from the pneumothorax. The arrows indicate the outer
free air under the diaphragm consistent with a perforated viscus. border of the right lung. The remainder of the right chest cavity is filled
(Film courtesy of Julie Takasugi, MD) with air in the pleural space. (Film courtesy of Julie Takasugi, MD)