Page 370 - Cardiac Nursing
P. 370
e 3
e 3
g
g
46
A
46
46
3-3
87.
33
3-3
q
q
87.
q
/30
6
/09
/30
g
xd
6
Pa
2:1
1
xd
2:1
/09
/09
1
1
M
M
Pa
c.
6 A
6 A
Pa
LWBK340-c16_
LWB
LWB K34 0-c 16_ p p pp333-387.qxd 6/30/09 12:16 AM Page 346 Aptara Inc.
16_
0-c
K34
c.
t
A
33
p
p
p
t
In
a
a
ara
ara
In
346 P A R T III / Assessment of Heart Disease
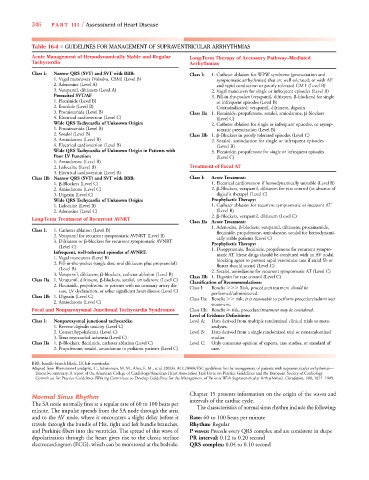
Table 16-4 ■ GUIDELINES FOR MANAGEMENT OF SUPRAVENTRICULAR ARRHYTHMIAS
Acute Management of Hemodynamically Stable and Regular Long-Term Therapy of Accessory Pathway–Mediated
Tachycardia Arrhythmias
Class I: Narrow QRS (SVT) and SVT with BBB: Class I: 1. Catheter ablation for WPW syndrome (preexcitation and
1. Vagal maneuvers (Valsalva, CSM) (Level B) symptomatic arrhythmias) that are well tolerated; or with AF
2. Adenosine (Level A) and rapid conduction or poorly tolerated CMT (Level B)
3. Verapamil, diltiazem (Level A) 2. Vagal maneuvers for single or infrequent episodes (Level B)
Preexcited SVT/AF 3. Pill-in-the-pocket (verapamil, diltiazem, -blockers) for single
1. Flecainide (Level B) or infrequent episodes (Level B)
2. Ibutilide (Level B) Contraindicated: verapamil, diltiazem, digoxin
3. Procainamide (Level B) Class IIa 1. Flecainide, propafenone, sotalol, amiodarone, -blockers
4. Electrical cardioversion (Level C) (Level C)
Wide QRS Tachycardia of Unknown Origin: 2. Catheter ablation for single or infrequent episodes, or asymp-
1. Procainamide (Level B) tomatic preexcitation (Level B)
2. Sotalol (Level B) Class IIb 1. -Blockers in poorly tolerated episodes (Level C)
3. Amiodarone (Level B) 2. Sotalol, amiodarone for single or infrequent episodes
4. Electrical cardioversion (Level B) (Level B)
Wide QRS Tachycardia of Unknown Origin in Patients with 3. Flecainide, propafenone for single or infrequent episodes
Poor LV Function: (Level C)
1. Amiodarone (Level B)
2. Lidocaine (Level B) Treatment of Focal AT
3. Electrical cardioversion (Level B)
Class IIb Narrow QRS (SVT) and SVT with BBB: Class I: Acute Treatment:
1. -Blockers (Level C) 1. Electrical cardioversion if hemodynamically unstable (Level B)
2. Amiodarone (Level C) 2. -Blockers, verapamil, diltiazem for rate control (in absence of
3. Digoxin (Level C) digitalis therapy) (Level C)
Wide QRS Tachycardia of Unknown Origin: Prophylactic Therapy:
1. Lidocaine (Level B) 1. Catheter ablation for recurrent symptomatic or incessant AT
2. Adenosine (Level C) (Level B)
2. -Blockers, verapamil, diltiazem (Level C)
Long-Term Treatment of Recurrent AVNRT
Class IIa Acute Treatment:
1. Adenosine, -blockers, verapamil, diltiazem, procainamide,
Class I: 1. Catheter ablation (Level B) flecainide, propafenone, amiodarone, sotalol for hemodynami-
2. Verapamil for recurrent symptomatic AVNRT (Level B) cally stable patients (Level C)
3. Diltiazem or -blockers for recurrent symptomatic AVNRT Prophylactic Therapy:
(Level C) 1. Disopyramide, flecainide, propafenone for recurrent sympto-
Infrequent, well-tolerated episodes of AVNRT: matic AT (these drugs should be combined with an AV nodal
1. Vagal maneuvers (Level B) blocking agent to prevent rapid ventricular rate if atrial fib or
2. Pill-in-the-pocket (single dose oral diltiazem plus propranolol) flutter should occur) (Level C)
(Level B) 2. Sotalol, amiodarone for recurrent symptomatic AT (Level C)
3. Verapamil, diltiazem, -blockers, catheter ablation (Level B) Class IIb 1. Digoxin for rate control (Level C)
Class IIa 1. Verapamil, diltiazem, -blockers, sotalol, amiodarone (Level C) Classification of Recommendations:
2. Flecainide, propafenone in patients with no coronary artery dis- Class I: Benefit Risk, procedure/treatment should be
ease, LV dysfunction, or other significant heart disease (Level C) performed/administered.
Class IIb 1. Digoxin (Level C) Class IIa: Benefit risk, it is reasonable to perform procedure/administer
2. Amiodarone (Level C)
treatment.
d
d
Focal and Nonparoxysmal Junctional Tachycardia Syndromes Class IIb: Benefit risk, procedure/treatment may be considered.
Level of Evidence Definitions:
Class I: Nonparoxysmal junctional tachycardia: Level A: Data derived from multiple randomized clinical trials or meta-
1. Reverse digitalis toxicity (Level C) analyses.
2. Correct hypokalemia (Level C) Level B: Data derived from a single randomized trial or nonrandomized
3. Treat myocardial ischemia (Level C) studies.
Class IIa 1. -Blockers, flecainide, catheter ablation (Level C) Level C: Only consensus opinion of experts, case studies, or standard of
2. Propafenone, sotalol, amiodarone in pediatric patients (Level C) care.
BBB, bundle-branch block; LV, left ventricular.
Adapted from Blomstrom-Lundqvist, C., Scheinman, M. M., Aliot, E. M., et al. (2003). ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias—
Executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology
Committee for Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Supraventricular Arrhythmias). Circulation, 108, 1871–1909.
r
Chapter 15 presents information on the origin of the waves and
Normal Sinus Rhythm
The SA node normally fires at a regular rate of 60 to 100 beats per intervals of the cardiac cycle.
minute. The impulse spreads from the SA node through the atria The characteristics of normal sinus rhythm include the following:
and to the AV node, where it encounters a slight delay before it Rate: 60 to 100 beats per minute
travels through the bundle of His, right and left bundle branches, Rhythm: Regular
and Purkinje fibers into the ventricles. The spread of this wave of P waves: Precede every QRS complex and are consistent in shape
depolarization through the heart gives rise to the classic surface PR interval: 0.12 to 0.20 second
electrocardiogram (ECG), which can be monitored at the bedside. QRS complex: 0.04 to 0.10 second