Page 2238 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 2238
Chapter 134 Thrombotic Thrombocytopenic Purpura and the Hemolytic Uremic Syndromes 1985
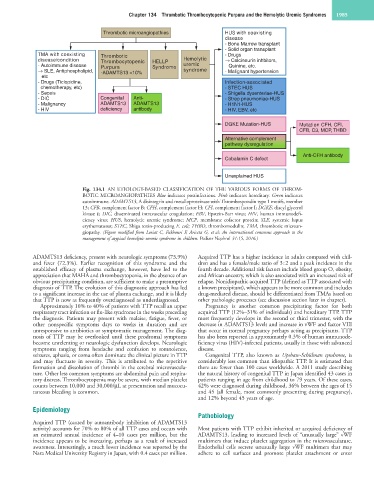
Thrombotic microangiopathies HUS with coexisting
disease
- Bone Marrow transplant
- Solid organ transplant
TMA with coexisting Thrombotic - Drugs
disease/condition Thrombocytopenic HELLP Hemolytic Calcineurin inhbitors,
- Autoimmune disease Purpura Syndrome uremic Quinine, etc.
SLE, Antiphospholipid, -ADAMTS13 <10% syndrome - Malignant hypertension
etc
- Drugs (Ticlopidine, Infection-associated
chemotherapy, etc) - STEC HUS
- Sepsis - Shigella dysenteriae-HUS
- DIC Congenital Anti- - Strep pneumoniae-HUS
- Malignancy ADAMTS13 ADAMTS13 - H1N1-HUS
- HIV deficiency antibody - HIV, EBV, etc
DGKE Mutation-HUS Mutation CFH, CFI,
CFB, C3, MCP, THBD
Alternative complement
pathway dysregulation
Anti-CFH antibody
Cobalamin C defect
Unexplained HUS
Fig. 134.1 AN ETIOLOGY-BASED CLASSIFICATION OF THE VARIOUS FORMS OF THROM-
BOTIC MICROANGIOPATHIES Blue indicates postinfectious. Pink indicates hereditary. Green indicates
autoimmune. ADAMTS13, A disintegrin and metalloproteinase with Thrombospondin type 1 motifs, member
13; CFB, complement factor B; CFH, complement factor H; CFI, complement factor I; DGKE, diacyl glycerol
kinase ε; DIC, disseminated intravascular coagulation; EBV, Epstein-Barr virus; HIV, human immunodefi-
ciency virus; HUS, hemolytic uremic syndrome; MCP, membrane cofactor protein; SLE, systemic lupus
erythematosus; STEC, Shiga toxin-producing E. coli; THBD, thrombomodulin; TMA, thrombotic microan-
giopathy. (Figure modified from Loriat C, Fakhouri F, Ariceta G, et al: An international consensus approach to the
management of atypical hemolytic uremic syndrome in children. Pediatr Nephrol 31:15, 2016.)
ADAMTS13 deficiency, present with neurologic symptoms (73.9%) Acquired TTP has a higher incidence in adults compared with chil-
and fever (72.3%). Earlier recognition of this syndrome and the dren and has a female/male ratio of 3 : 2 and a peak incidence in the
established efficacy of plasma exchange, however, have led to the fourth decade. Additional risk factors include blood group O, obesity,
appreciation that MAHA and thrombocytopenia, in the absence of an and African ancestry, which is also associated with an increased risk of
obvious precipitating condition, are sufficient to make a presumptive relapse. Nonidiopathic acquired TTP (defined as TTP associated with
diagnosis of TTP. The evolution of this diagnostic approach has led a known precipitant), which appears to be more common and includes
to a significant increase in the use of plasma exchange, and it is likely drug-mediated disease, should be differentiated from TMAs based on
that TTP is now as frequently overdiagnosed as underdiagnosed. other pathologic processes (see discussion section later in chapter).
Approximately 10% to 40% of patients with TTP recall an upper Pregnancy is another common precipitating factor for both
respiratory tract infection or flu-like syndrome in the weeks preceding acquired TTP (12%–31% of individuals) and hereditary TTP. TTP
the diagnosis. Patients may present with malaise, fatigue, fever, or most frequently develops in the second or third trimester, with the
other nonspecific symptoms days to weeks in duration and are decrease in ADAMTS13 levels and increase in vWF and factor VIII
unresponsive to antibiotics or symptomatic management. The diag- that occur in normal pregnancy perhaps acting as precipitants. TTP
nosis of TTP may be overlooked until these prodromal symptoms has also been reported in approximately 0.3% of human immunode-
become unrelenting or neurologic dysfunction develops. Neurologic ficiency virus (HIV)-infected patients, usually in those with advanced
symptoms ranging from headache and confusion to somnolence, disease.
seizures, aphasia, or coma often dominate the clinical picture in TTP Congenital TTP, also known as Upshaw-Schülman syndrome, is
and may fluctuate in severity. This is attributed to the repetitive considerably less common than idiopathic TTP. It is estimated that
formation and dissolution of thrombi in the cerebral microvascula- there are fewer than 100 cases worldwide. A 2011 study describing
ture. Other less common symptoms are abdominal pain and respira- the natural history of congenital TTP in Japan identified 43 cases in
tory distress. Thrombocytopenia may be severe, with median platelet patients ranging in age from childhood to 79 years. Of these cases,
counts between 10,000 and 30,000/µL at presentation and mucocu- 42% were diagnosed during childhood, 36% between the ages of 15
taneous bleeding is common. and 45 (all female, most commonly presenting during pregnancy),
and 12% beyond 45 years of age.
Epidemiology
Pathobiology
Acquired TTP (caused by autoantibody inhibition of ADAMTS13
activity) accounts for 70% to 80% of all TTP cases and occurs with Most patients with TTP exhibit inherited or acquired deficiency of
an estimated annual incidence of 4–10 cases per million, but the ADAMTS13, leading to increased levels of “unusually large” vWF
incidence appears to be increasing, perhaps as a result of increased multimers that induce platelet aggregation in the microvasculature.
awareness. Interestingly, a much lower incidence was reported by the Endothelial cells secrete unusually large vWF multimers that may
Nara Medical University Registry in Japan, with 0.4 cases per million. adhere to cell surfaces and promote platelet attachment or enter