Page 2258 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 2258
Chapter 135 Hemophilia A and B 2005
NH2 COOH HNF4
DBP AR COUP-TF
SP PrP Gla EGF1 EGF2 AP Catalytic C/EBP HNF4 ARP C/EBP
CC
1 145 180 415 5′ 4 3 2 1 F9
gene
FXIa and/or FVIIa-TF –220 –190
Gla EGF1 EGF2 Catalytic –26 –21 –6 +6 +11
–20 –5 +8
–19
CC
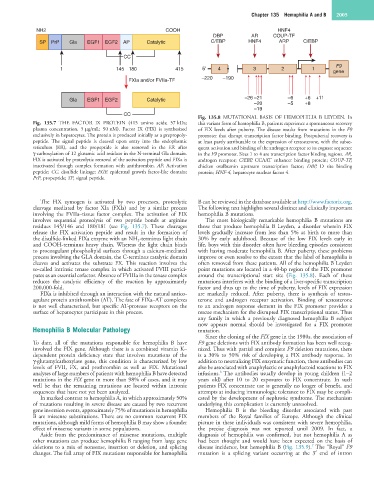
Fig. 135.8 MUTATIONAL BASIS OF HEMOPHILIA B LEYDEN. In
Fig. 135.7 THE FACTOR IX PROTEIN (415 amino acids; 57 kDa; this variant form of hemophilia B, patients experience a spontaneous recovery
plasma concentration, 5 µg/mL; 90 nM). Factor IX (FIX) is synthesized of FIX levels after puberty. The disease results from mutations in the F9
exclusively in hepatocytes. The protein is produced initially as a prepropoly- promoter that disrupt transcription factor binding. Postpubertal recovery is
peptide. The signal peptide is cleaved upon entry into the endoplasmic at least partly attributable to the expression of testosterone, with the subse-
reticulum (ER), and the propeptide is also removed in the ER after quent activation and binding of the androgen receptor to its cognate sequence
γ-carboxylation of 12 glutamic acid residues in the N-terminal Gla domain. in the F9 promoter. Sites 1 to 4 are transcription factor binding regions. AR,
FIX is activated by proteolytic removal of the activation peptide and FIXa is androgen receptor; C/EBP, CCAAT enhancer binding protein; COUP-TF,
inactivated through complex formation with antithrombin. AP, Activation chicken ovalbumin upstream transcription factor; DBP, D site binding
peptide; CC, disulfide linkage; EGF, epidermal growth factor-like domain; protein; HNF-4, hepatocyte nuclear factor 4.
PrP, propeptide; SP, signal peptide.
The FIX zymogen is activated by two processes, proteolytic B can be reviewed in the database available at http://www.factorix.org.
cleavage mediated by factor XIa (FXIa) and by a similar process The following text highlights several distinct and clinically important
involving the FVIIa–tissue factor complex. The activation of FIX hemophilia B mutations.
involves sequential proteolysis of two peptide bonds at arginine The most biologically remarkable hemophilia B mutations are
residues 145/146 and 180/181 (see Fig. 135.7). These cleavages those that produce hemophilia B Leyden, a disorder wherein FIX
release the FIX activation peptide and result in the formation of levels gradually increase from less than 5% at birth to more than
the disulfide-linked FIXa enzyme with an NH 2 -terminus light chain 30% by early adulthood. Because of the low FIX levels early in
and COOH-terminus heavy chain. Whereas the light chain binds life, boys with this disorder often have bleeding episodes consistent
to procoagulant phospholipid surfaces through a calcium-mediated with having moderate hemophilia B. After puberty, these problems
process involving the GLA domain, the C-terminus catalytic domain improve or even resolve to the extent that the label of hemophilia is
cleaves and activates the substrate FX. This reaction involves the often removed from these patients. All of the hemophilia B Leyden
so-called intrinsic tenase complex in which activated FVIII partici- point mutations are located in a 40-bp region of the FIX promoter
pates as an essential cofactor. Absence of FVIIIa in the tenase complex around the transcriptional start site (Fig. 135.8). Each of these
reduces the catalytic efficiency of the reaction by approximately mutations interferes with the binding of a liver-specific transcription
200,000-fold. factor and thus up to the time of puberty, levels of FIX expression
FIXa is inhibited through an interaction with the natural antico- are markedly reduced. After puberty, there is synthesis of testos-
agulant protein antithrombin (AT). The fate of FIXa–AT complexes terone and androgen receptor activation. Binding of testosterone
is not well characterized, but specific AT-protease receptors on the to an androgen response element in the FIX promoter provides a
surface of hepatocytes participate in this process. rescue mechanism for the disrupted FIX transcriptional status. Thus
any family in which a previously diagnosed hemophilia B subject
now appears normal should be investigated for a FIX promoter
Hemophilia B Molecular Pathology mutation.
Since the cloning of the FIX gene in the 1980s, the association of
To date, all of the mutations responsible for hemophilia B have F9 gene deletions with FIX antibody formation has been well recog-
involved the FIX gene. Although there is a combined vitamin K– nized. Thus with partial and complete F9 deletion mutations, there
dependent protein deficiency state that involves mutations of the is a 30% to 50% risk of developing a FIX antibody response. In
γ-glutamylcarboxylase gene, this condition is characterized by low addition to neutralizing FIX enzymatic function, these antibodies can
levels of FVII, FX, and prothrombin as well as FIX. Mutational also be associated with anaphylactic or anaphylactoid reactions to FIX
6
analyses of large numbers of patients with hemophilia B have detected infusions. The antibodies usually develop in young children (1–2
mutations in the FIX gene in more than 98% of cases, and it may years old) after 10 to 20 exposures to FIX concentrate. In such
well be that the remaining mutations are located within intronic patients FIX concentrate use is generally no longer of benefit, and
sequences that have not yet been analyzed. attempts at inducing immunologic tolerance to FIX may be compli-
In marked contrast to hemophilia A, in which approximately 50% cated by the development of nephrotic syndrome. The mechanism
of mutations resulting in severe disease are caused by two recurrent underlying this complication is currently unresolved.
gene inversion events, approximately 75% of mutations in hemophilia Hemophilia B is the bleeding disorder associated with past
B are missense substitutions. There are no common recurrent FIX members of the Royal families of Europe. Although the clinical
mutations, although mild forms of hemophilia B may show a founder picture in these individuals was consistent with severe hemophilia,
effect of missense variants in some populations. the precise diagnosis was not reported until 2009. In fact, a
Aside from the predominance of missense mutations, multiple diagnosis of hemophilia was confirmed, but not hemophilia A as
other mutations can produce hemophilia B ranging from large gene had been thought and would have been expected on the basis of
7
deletions to a mix of nonsense, insertion or deletion, and splicing disease incidence, but hemophilia B (Fig. 135.9). The “Royal” F9
changes. The full array of FIX mutations responsible for hemophilia mutation is a splicing variant occurring at the 3′ end of intron