Page 415 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 415
CHAPTER 36: Cardiac Arrhythmias, Pacing, Cardioversion, and Defibrillation in the Critical Care Setting 285
Synchronized cardioversion with 120 to 200 J biphasic shock (depending therapy. 33-35 In patients with less severe left ventricular dysfunction, ami-
on manufacturer’s recommendation) or 360 J monophasic shock is the odarone appears to be as efficacious as the ICD and long-term therapy
initial approach for the patient with hemodynamically unstable V . If the with amiodarone or an ICD may be individualized. 35
t
patient is hemodynamically stable and has normal or only mild left ven-
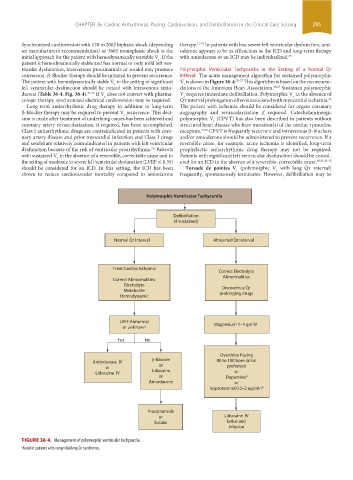
tricular dysfunction, intravenous procainamide or sotalol may promote Polymorphic Ventricular Tachycardia in the Setting of a Normal Q ˙ t
conversion. β-Blocker therapy should be initiated to prevent recurrence. Interval: The acute management algorithm for sustained polymorphic
The patient with hemodynamically stable V in the setting of significant V is shown in Figure 36-4. 25-27 This algorithm is based on the recommen-
t
t
left ventricular dysfunction should be treated with intravenous amio- dations of the American Heart Association. 26,27 Sustained polymorphic
darone (Table 36-4, Fig. 36-4). 25-27 If V does not convert with pharma- V requires immediate defibrillation. Polymorphic V in the absence of
t
t
t
cologic therapy, synchronized electrical cardioversion may be required. Q ˙ t interval prolongation often is associated with myocardial ischemia.
23
Long-term antiarrhythmic drug therapy in addition to long-term The patient with ischemia should be considered for urgent coronary
β-blocker therapy may be required to prevent V recurrence. This deci- angiography and revascularization if required. Catecholaminergic
t
sion is made after treatment of underlying causes has been achieved and polymorphic V (CPVT) has also been described in patients without
t
coronary artery revascularization, if required, has been accomplished. structural heart disease who have mutation(s) of the cardiac ryanodine
Class I antiarrhythmic drugs are contraindicated in patients with coro- receptors. 24,36 CPVT is frequently recurrent and intravenous β-blockers
nary artery disease and prior myocardial infarction and Class I drugs and/or amiodarone should be administered to prevent recurrence. If a
and sotalol are relatively contraindicated in patients with left ventricular reversible cause, for example, acute ischemia is identified, long-term
dysfunction because of the risk of ventricular proarrhythmia. Patients prophylactic antiarrhythmic drug therapy may not be required.
7,8
with sustained V in the absence of a reversible, correctable cause and in Patients with significant left ventricular dysfunction should be consid-
t
the setting of moderate to severe left ventricular dysfunction (LVEF ≤ 0.35) ered for an ICD in the absence of a reversible, correctable cause. 30,31,33-35
should be considered for an ICD. In this setting, the ICD has been Torsade de pointes V (polymorphic V with long Q ˙ t interval)
t
t
shown to reduce cardiovascular mortality compared to amiodarone frequently, spontaneously terminates. However, defibrillation may be
Polymorphic Ventricular Tachycardia
Defibrillation
(if sustained)
Normal QT Interval Abnormal QT Interval
Treat Cardiac Ischemia
Correct Electrolyte
Abnormalities
Correct Abnormalities:
Electrolyte
Discontinue QT
Metabolite prolonging drugs
Hemodynamic
LVEF Abnormal Magnesium 1–4 gm IV
or unknown
Yes No
Overdrive Pacing
β-blocker
Amiodarone IV 80 to 100 bpm (atrial
or or preferred)
Lidocaine IV Lidocaine or
or Dopamine a
Amiodarone or
Isoproterenol 0.5–2 ug/min a
Procainamide
or Lidocaine IV
Sotalol bolus and
infusion
FIGURE 36-4. Management of polymorphic ventricular tachycardia.
a Avoid in patients with congenital long Q t syndromes.
˙
section03.indd 285 1/23/2015 2:07:11 PM