Page 414 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 414
284 PART 3: Cardiovascular Disorders
causes should be identified and corrected (Table 36-7). 25-27 The TABLE 36-7 Management of Ventricular Tachycardia due to Reversible Causes
serum potassium should be maintained ≥4.0 mM/L and the serum
magnesium should be maintained >0.7 mM/L. β-Blockers should be Cause Management
prescribed unless contraindicated (Table 36-4). Management of isch- Acute ischemia/myocardial infarction Amiodarone and/or β-blockers,
emic heart disease, left ventricular dysfunction and/or hypertension revascularization
must be optimized. If ongoing ischemia/cardiogenic shock is present
despite medical therapy, the patient should be considered for urgent Congestive heart failure Optimize therapy of CHF,
coronary artery evaluation and possible revascularization. ACE inhibitors,
Nonsustained V : β-Blockers should be prescribed unless contrain- β-blockers,
T
dicated and doses should be titrated to suppress nonsustained V
t
(Table 36-4). 17,25,28,29 If frequent, hemodynamically significant nonsus- consider ICD
tained V persists, amiodarone may be initiated for suppression. 17,25-27,30 Electrolyte abnormalities (usually torsade de MgSO 1-4 g IV, KC1, atrial overdrive
4
t
Patients with mild to moderate left ventricular dysfunction (left pointes V ) pacing
t
ventricular ejection fraction [LVEF] >0.30) may be considered for Drug toxicity/long Qt (torsade de pointes V ) MgSO 1-4 g IV, atrial overdrive pacing
˙
a risk stratification electrophysiology study to determine the risk of t (80-100 bpm), discontinue
4
sudden cardiac death. 16,30 Patients with severe left ventricular dysfunc- class I/III drugs
tion in the setting of ischemic heart disease (LVEF ≤ 0.30) or dilated
cardiomyopathy should be considered for an implantable cardioverter Drug toxicity (incessant monomorphic V, Sodium bicarbonate (50-200 meq IV),
t
defibrillator (ICD) for prophylaxis of sudden cardiac death. 21,31,32 eg, flecainide/propafenone/tricyclic antidepressants) lidocaine (0.5-0.75 mg/kg)
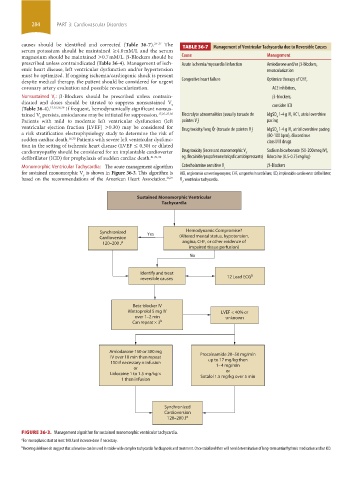
Monomorphic Ventricular Tachycardia: The acute management algorithm Catecholamine sensitive V t β-Blockers
for sustained monomorphic V is shown in Figure 36-3. This algo rithm is ACE, angiotensin converting enzyme; CHF, congestive heart failure; ICD, implantable cardioverter defibrillator;
t
based on the recommendations of the American Heart Association. 26,27 V , ventricular tachycardia.
t
Sustained Monomorphic Ventricular
Tachycardia
Synchronized Yes Hemodynamic Compromise?
Cardioversion (Altered mental status, hypotension,
120–200 J a angina, CHF, or other evidence of
impaired tissue perfusion)
No
Identify and treat b
reversible causes 12 Lead ECG
Beta-blocker IV
Metroprolol 5 mg IV LVEF < 40% or
over 1–2 min unknown
Can repeat × 3 b
Amiodarone 150 or 300 mg Procainamide 20–50 mg/min
IV over 10 min then repeat up to 17 mg/kg then
150 if necessary ± infusion
or 1–4 mg/min
Lidocaine 1 to 1.5 mg/kg × or
1 then infusion Sotalol 1.5 mg/kg over 5 min
Synchronized
Cardioversion
120–200 J a
FIGURE 36-3. Management algorithm for sustained monomorphic ventricular tachycardia.
a For monophasic start at least 100 J and increase dose if necessary.
b Recent guidelines do suggest that adenosine can be used in stable wide complex tachycardia for diagnosis and treatment. Once stabilized then will need determination of long-term antiarrhythmic medication and/or ICD.
section03.indd 284 1/23/2015 2:07:11 PM