Page 416 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 416
286 PART 3: Cardiovascular Disorders
required if it becomes sustained. Magnesium 1 to 4 g intravenously is the for prevention of sudden cardiac death should be prescribed. Patients
initial treatment followed by cardiac overdrive pacing at 80 to 100 bpm, with VF should be considered for an ICD, although in patients with
which shortens the Q ˙ t interval and prevents long pauses following pre- well-preserved left ventricular dysfunction, amiodarone may also be
mature beats (Fig. 36-4). 25,37 Atrial overdrive pacing is preferred to ven- a reasonable treatment option. 31,33-35,39
tricular overdrive pacing. An isoproterenol infusion, with dose titrated to
achieve a heart rate of 80 to 100 bpm, may be started until a temporary V /VF Electrical Storm: This is defined as multiple recurrent (usually
T
pacemaker is inserted. Drugs causing Q ˙ t interval prolongation should >3) episodes of sustained V or VF within a 24-hour period. Reversible
t
be stopped and any electrolyte imbalances corrected. Temporary pacing causes should be identified and treated (Table 36-4). β-Blockers are
25,28
should be continued until the V has subsided and the Q ˙ t interval returns effective in suppressing some episodes of V /VF storm. Even in
t
t
to normal. If the patient has congenital long Q ˙ t syndrome, long-term the setting of congestive heart failure (except cardiogenic shock), intra-
prophylactic therapy with β-blockers and/or permanent atrial pacing will venous β-blockers can be safely administered. Amiodarone is very effec-
prevent torsade de pointes V . 21,38 An ICD is the treatment of choice in tive in suppressing V /VF although multiple boluses may be required
t
30
t
patients with congenital long Q ˙ t syndrome who have sustained a cardiac in some patients. Combination β-blocker and amiodarone therapy is
25
arrest or who have a significant family history of sudden cardiac death. 21 likely synergistic in suppressing recurrent V /VF. In the patient with
t
an ICD and V electrical storm who is receiving frequent, painful shock
t
Ventricular Fibrillation and Pulseless V : Advanced life support should be therapies, if the V is relatively stable, then cardioversion/defibrilla-
t
T
initiated for VF (or pulseless V ), with prompt CPR and defibrillation tion therapies may need to be temporarily programmed off (antitachycardia
t
(Fig. 36-5). 25-27 If the first defibrillation is unsuccessful then vasopres- pacing therapies can be left on and/or modified) until pharmacologic
sor (epinephrine or vasopressin) therapy should be given. Amiodarone therapy suppresses the frequency of V . In some patients, especially
t
(lidocaine if amiodarone not available) should be initiated when VF is those with prior amiodarone toxicity, lidocaine, or procainamide will
refractory to shocks, CPR, and vasopressor treatments. Intravenous be necessary to suppress V . Addition of anxiolytics and narcotics can
26
t
amiodarone has been shown to improve resuscitation rates and overall help with anxiety as well as further helping to reduce the adrenergic
survival if initial defibrillation is unsuccessful. If acute myocardial stimulus. Patients in V storm who are refractory to the above mea-
t
ischemia is the cause of VF, coronary angiography and percutane- sures may require sedation, paralysis, intubation, and ventilation to
ous coronary intervention should be considered in the patient with further help with their acute V management.
t
recurrent VF. In the absence of a reversible cause, long-term therapy
SUPRAVENTRICULAR TACHYARRHYTHMIAS
■
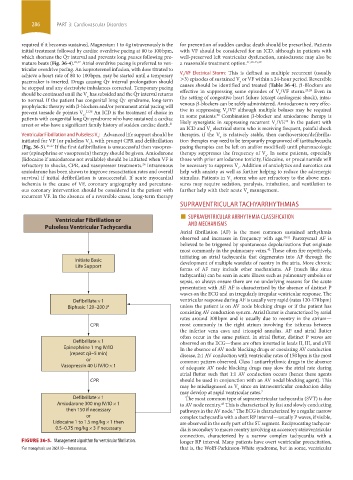
Ventricular Fibrillation or SUPRAVENTRICULAR ARRHYTHMIA CLASSIFICATION
Pulseless Ventricular Tachycardia AND MECHANISMS
Atrial fibrillation (AF) is the most common sustained arrhythmia
observed and increases in frequency with age. 40,41 Paroxysmal AF is
believed to be triggered by spontaneous depolarizations that originate
most commonly in the pulmonary veins. These often fire repetitively,
42
initiating an atrial tachycardia that degenerates into AF through the
Initiate Basic development of multiple wavelets of reentry in the atria. More chronic
Life Support
forms of AF may include other mechanisms. AF (much like sinus
tachycardia) can be seen in acute illness such as pulmonary embolus or
sepsis, so always ensure there are no underlying reasons for the acute
presentation with AF. AF is characterized by the absence of distinct P
waves on the ECG and an irregularly irregular ventricular response. The
Defibrillate × 1 ventricular response during AF is usually very rapid (rates 120-170 bpm)
Biphasic 120–200 J a unless the patient is on AV node blocking drugs or if the patient has
coexisting AV conduction system. Atrial flutter is characterized by atrial
rates around 300 bpm and is usually due to reentry in the atrium—
CPR most commonly in the right atrium involving the isthmus between
the inferior vena cava and tricuspid annulus. AF and atrial flutter
often occur in the same patient. In atrial flutter, distinct P waves are
Defibrillate × 1 observed on the ECG—these are often inverted in leads II, III, and aVF.
Epinephrine 1 mg IV/IO In the absence of AV node blocking drugs or coexisting AV conduction
(repeat q3–5 min) disease, 2:1 AV conduction with ventricular rates of 150 bpm is the most
or common pattern observed. Class I antiarrhythmic drugs in the absence
Vasopressin 40 U IV/IO × 1 of adequate AV node blocking drugs may slow the atrial rate during
atrial flutter such that 1:1 AV conduction occurs (hence these agents
CPR should be used in conjunction with an AV nodal blocking agent). This
may be misdiagnosed as V since an intraventricular conduction delay
t
may develop at rapid ventricular rates. 7
Defibrillate × 1 The most common type of supraventricular tachycardia (SVT) is due
Amiodarone 300 mg IV/IO × 1 to AV node reentry. This is characterized by fast and slowly conducting
43
then 150 if necessary pathways in the AV node. The ECG is characterized by a regular narrow
2
or complex tachycardia with a short RP interval—usually P waves, if visible,
Lidocaine 1 to 1.5 mg/kg × 1 then are observed in the early part of the ST segment. Reciprocating tachycar-
0.5–0.75 mg/kg × 3 if necessary dia is secondary to macro reentry involving an accessory atrioventricular
connection, characterized by a narrow complex tachycardia with a
FIGURE 36-5. Management algorithm for ventricular fibrillation. longer RP interval. Many patients have overt ventricular preexcitation,
a For monophasic use 360J. IO—Intraosseous. that is, the Wolff-Parkinson-White syndrome, but in some, ventricular
section03.indd 286 1/23/2015 2:07:12 PM