Page 83 - The Netter Collection of Medical Illustrations - Integumentary System_ Volume 4 ( PDFDrive )
P. 83
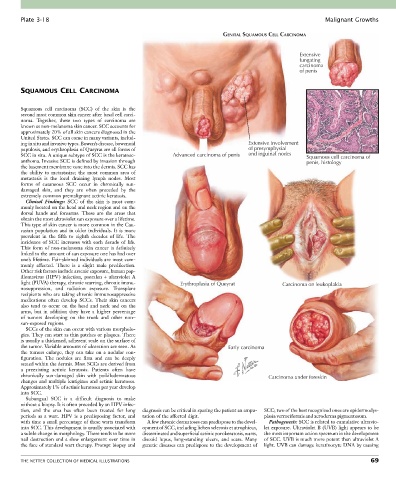
Plate 3-18 Malignant Growths
GENITAL SQUAMOUS CELL CARCINOMA
Extensive
fungating
carcinoma
of penis
SQUAMOUS CELL CARCINOMA
Squamous cell carcinoma (SCC) of the skin is the
second most common skin cancer after basal cell carci-
noma. Together, these two types of carcinoma are
known as non-melanoma skin cancer. SCC accounts for
approximately 20% of all skin cancers diagnosed in the
United States. SCC can come in many variants, includ-
ing in situ and invasive types. Bowen’s disease, bowenoid Extensive involvement
papulosis, and erythroplasia of Queyrat are all forms of of presymphysial
SCC in situ. A unique subtype of SCC is the keratoac- Advanced carcinoma of penis and inguinal nodes Squamous cell carcinoma of
anthoma. Invasive SCC is defined by invasion through penis, histology
the basement membrane zone into the dermis. SCC has
the ability to metastasize; the most common area of
metastasis is the local draining lymph nodes. Most
forms of cutaneous SCC occur in chronically sun-
damaged skin, and they are often preceded by the
extremely common premalignant actinic keratosis.
Clinical Findings: SCC of the skin is most com-
monly located on the head and neck region and on the
dorsal hands and forearms. These are the areas that
obtain the most ultraviolet sun exposure over a lifetime.
This type of skin cancer is more common in the Cau-
casian population and in older individuals. It is more
prevalent in the fifth to eighth decades of life. The
incidence of SCC increases with each decade of life.
This form of non-melanoma skin cancer is definitely
linked to the amount of sun exposure one has had over
one’s lifetime. Fair-skinned individuals are most com-
monly affected. There is a slight male predilection.
Other risk factors include arsenic exposure, human pap-
illomavirus (HPV) infection, psoralen + ultraviolet A
light (PUVA) therapy, chronic scarring, chronic immu- Erythroplasia of Queyrat Carcinoma on leukoplakia
nosuppression, and radiation exposure. Transplant
recipients who are taking chronic immunosuppressive
medications often develop SCCs. Their skin cancers
also tend to occur on the head and neck and on the
arms, but in addition they have a higher percentage
of tumors developing on the trunk and other non–
sun-exposed regions.
SCCs of the skin can occur with various morpholo-
gies. They can start as thin patches or plaques. There
is usually a thickened, adherent scale on the surface of
the tumor. Variable amounts of ulceration are seen. As Early carcinoma
the tumors enlarge, they can take on a nodular con-
figuration. The nodules are firm and can be deeply
seated within the dermis. Most SCCs are derived from
a preexisting actinic keratosis. Patients often have
chronically sun-damaged skin with poikilodermatous Carcinoma under foreskin
changes and multiple lentigines and actinic keratoses.
Approximately 1% of actinic keratoses per year develop
into SCC.
Subungual SCC is a difficult diagnosis to make
without a biopsy. It is often preceded by an HPV infec-
tion, and the area has often been treated for long diagnosis can be critical in sparing the patient an ampu- SCC; two of the best recognized ones are epidermodys-
periods as a wart. HPV is a predisposing factor, and tation of the affected digit. plasia verruciformis and xeroderma pigmentosum.
with time a small percentage of these warts transform A few chronic dermatoses can predispose to the devel- Pathogenesis: SCC is related to cumulative ultravio-
into SCC. This development is usually associated with opment of SCC, including lichen sclerosis et atrophicus, let exposure. Ultraviolet B (UVB) light appears to be
a subtle change in morphology. There tends to be more disseminated and superficial actinic porokeratosis, warts, the most important action spectrum in the development
nail destruction and a slow enlargement over time in discoid lupus, long-standing ulcers, and scars. Many of SCC. UVB is much more potent than ultraviolet A
the face of standard wart therapy. Prompt biopsy and genetic diseases can predispose to the development of light. UVB can damage keratinocyte DNA by causing
THE NETTER COLLECTION OF MEDICAL ILLUSTRATIONS 69