Page 246 - Cardiac Nursing
P. 246
009
1
6/2
009
1
6 A
6 A
0:4
0:4
6/2
q
xd
q
q
xd
0/0
0/0
3
3
M
p
p
A
A
p
ara
ara
t
t
22
Pa
g
M
Pa
g
e 2
22
g
e 2
LWBK340-c10_
21
21
0-c
K34
LWB
10_
1-2
44.
44.
LWB K34 0-c 10_ p p pp211-244.qxd 30/06/2009 10:46 AM Page 222 Aptara
1-2
222 P A R T III / Assessment of Heart Disease
Pulsus parvus et tardus (Fig. 10-6H) is found in severe aortic and ulnar arterial patency. Simultaneously compress the radial and
stenosis. It resembles the double systolic beat in pulsus bisferiens, ulnar arteries and ask the patient to make a fist. The hand blanches.
but its upstroke is more gradual and the pulse pressure is smaller. Ask the patient to open his or her fist. Release the pressure from
Usually it is palpable only in the carotid artery. the ulnar artery while maintaining pressure on the radial artery.
The hand color returns to normal if the ulnar artery is patent. Re-
Carotid Pulse. The carotid artery is best for assessing pulse-
peat the process releasing pressure from the radial artery. If dual cir-
wave amplitude and contour. Observe the neck for pulsations.
culation to the hand is not present, do not attempt radial arterial
Carotid pulsations are visible bilaterally just medial to the stern-
puncture or cannulation.
ocleidomastoid muscle. Place your fingertips along the medial bor-
In shock states associated with reduced cardiac output and el-
der of the sternocleidomastoid muscle in the lower half of the neck.
evated systemic vascular resistance, or with arterial insufficiency,
Press posteriorly to feel the artery. Palpate well below the upper
pulses may not be palpable in the periphery. In this case, Doppler
border of the thyroid cartilage to avoid compressing the carotid si-
ultrasound should be used to evaluate arterial flow. Using light
nus, which might result in a reflex drop in heart rate or blood pres-
pressure so that the artery is not occluded, place the Doppler
sure. Compare one side with the other, but do not palpate both
probe (with conducting gel) over the general area of the artery to
sides simultaneously because brain blood flow might be inter-
be assessed. Move the probe until the arterial signal is audible.
rupted. Using the side with the strongest pulsations, assess the am-
Mark the location of the pulse with indelible ink.
plitude and contour of the pulse wave and determine whether it
occurs in early systole or has a delayed upstroke.
Bruits
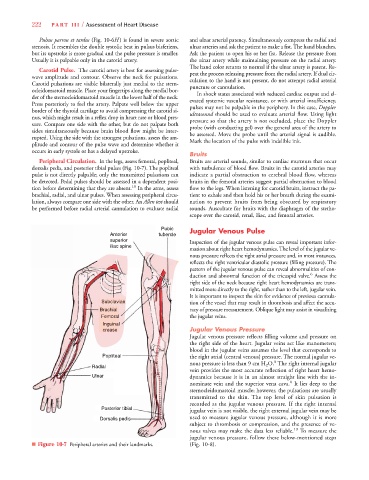
Peripheral Circulation. In the legs, assess femoral, popliteal, Bruits are arterial sounds, similar to cardiac murmurs that occur
dorsalis pedis, and posterior tibial pulses (Fig. 10-7). The popliteal with turbulence of blood flow. Bruits in the carotid arteries may
pulse is not directly palpable; only the transmitted pulsations can indicate a partial obstruction to cerebral blood flow, whereas
be detected. Pedal pulses should be assessed in a dependent posi- bruits in the femoral arteries suggest partial obstruction to blood
tion before determining that they are absent. 18 In the arms, assess flow to the legs. When listening for carotid bruits, instruct the pa-
brachial, radial, and ulnar pulses. When assessing peripheral circu- tient to exhale and then hold his or her breath during the exami-
lation, always compare one side with the other. An Allen test should nation to prevent bruits from being obscured by respiratory
be performed before radial arterial cannulation to evaluate radial sounds. Auscultate for bruits with the diaphragm of the stetho-
scope over the carotid, renal, iliac, and femoral arteries.
Pubic Jugular Venous Pulse
Anterior tubercle
superior Inspection of the jugular venous pulse can reveal important infor-
iliac spine
mation about right heart hemodynamics. The level of the jugular ve-
nous pressure reflects the right atrial pressure and, in most instances,
reflects the right ventricular diastolic pressure (filling pressure). The
pattern of the jugular venous pulse can reveal abnormalities of con-
6
duction and abnormal function of the tricuspid valve. Assess the
right side of the neck because right heart hemodynamics are trans-
mitted more directly to the right, rather than to the left, jugular vein.
It is important to inspect the skin for evidence of previous cannula-
Subclavian tion of the vessel that may result in thrombosis and affect the accu-
Brachial racy of pressure measurement. Oblique light may assist in visualizing
Femoral the jugular veins.
Inguina l
crease Jugular Venous Pressure
Jugular venous pressure reflects filling volume and pressure on
the right side of the heart. Jugular veins act like manometers;
blood in the jugular veins assumes the level that corresponds to
Pop the right atrial (central venous) pressure. The normal jugular ve-
pliteal
8
nous pressure is less than 9 cm H 2 O. The right internal jugular
Radial
vein provides the most accurate reflection of right heart hemo-
Ulnar dynamics because it is in an almost straight line with the in-
8
nominate vein and the superior vena cava. It lies deep to the
sternocleidomastoid muscle; however, the pulsations are usually
transmitted to the skin. The top level of skin pulsation is
recorded as the jugular venous pressure. If the right internal
Posterior tibial
jugular vein is not visible, the right external jugular vein may be
Dorsalis pedis s used to measure jugular venous pressure, although it is more
subject to thrombosis or compression, and the presence of ve-
nous valves may make the data less reliable. 19 To measure the
jugular venous pressure, follow these below-mentioned steps
■ Figure 10-7 Peripheral arteries and their landmarks. (Fig. 10-8).