Page 340 - Cardiac Nursing
P. 340
1
1
/09
/29
/09
0:3
M
M
0 P
0:3
0 P
/29
32.
q
32.
0-3
0-3
q
6
6
xd
q
xd
Pa
ara
ara
t
p
t
a
c.
c.
In
a
In
p
g
e 3
g
Pa
g
e 3
A
p
A
16
16
30
LWB K34 0-c 15_ pp300-332.qxd 6/29/09 10:30 PM Page 316 Aptara Inc.
p
LWB
LWBK340-c15_
0-c
p
15_
30
K34
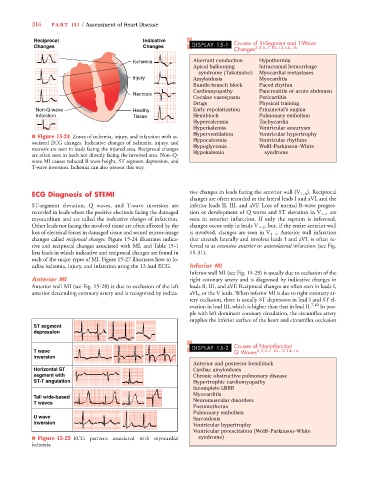
316 P A R T III / Assessment of Heart Disease
Reciprocal Indicative Causes of St-Segment and T-Wave
g
g
Changes Changes DISPLAY 15-1 2,3,5–7,10–12,14–16
Changes
Ischemia Aberrant conduction Hypothermia
Apical ballooning Intracranial hemorrhage
syndrome (Takotsubo) Myocardial metastases
Injury Amyloidosis Myocarditis
Bundle-branch block Paced rhythm
Cardiomyopathy Pancreatitis or acute abdomen
Necrosis
Cocaine vasospasm Pericarditis
Drugs Physical training
Non-Q-wave Healthy Early repolarization Prinzmetal’s angina
Infarction Tissue Hemiblock Pulmonary embolism
Hypercalcemia Tachycardia
Hyperkalemia Ventricular aneurysm
Hyperventilation Ventricular hypertrophy
■ Figure 15-24 Zones of ischemia, injury, and infarction with as-
sociated ECG changes. Indicative changes of ischemia, injury, and Hypocalcemia Ventricular rhythms
Hypoglycemia
Wolff–Parkinson–White
necrosis are seen in leads facing the injured area. Reciprocal changes Hypokalemia syndrome
are often seen in leads not directly facing the involved area. Non–Q-
wave MI causes reduced R wave height, ST segment depression, and
T-wave inversion. Ischemia can also present this way.
ECG Diagnosis of STEMI tive changes in leads facing the anterior wall (V 1–4 ). Reciprocal
changes are often recorded in the lateral leads I and aVL and the
ST-segment elevation, Q waves, and T-wave inversion are inferior leads II, III, and aVF. Loss of normal R-wave progres-
recorded in leads where the positive electrode facing the damaged sion or development of Q waves and ST elevation in V 1–4 are
myocardium and are called the indicative changes of infarction. seen in anterior infarction. If only the septum is infarcted,
Other leads not facing the involved tissue are often affected by the changes occur only in leads V 1–2 , but, if the entire anterior wall
loss of electrical forces in damaged tissue and record mirror-image is involved, changes are seen in V 1–4 . Anterior wall infarction
changes called reciprocal changes. Figure 15-24 illustrates indica- that extends laterally and involves leads I and aVL is often re-
tive and reciprocal changes associated with MI, and Table 15-1 ferred to as extensive anterior or anterolateral infarction (see Fig.
lists leads in which indicative and reciprocal changes are found in 15-31).
each of the major types of MI. Figure 15-27 illustrates how to lo-
calize ischemia, injury, and infarction using the 12-lead ECG. Inferior MI
Inferior wall MI (see Fig. 15-29) is usually due to occlusion of the
Anterior MI right coronary artery and is diagnosed by indicative changes in
Anterior wall MI (see Fig. 15-28) is due to occlusion of the left leads II, III, and aVF. Reciprocal changes are often seen in leads I,
anterior descending coronary artery and is recognized by indica- aVL, or the V leads. When inferior MI is due to right coronary ar-
tery occlusion, there is usually ST depression in lead I and ST el-
evation in lead III, which is higher than that in lead II. 7,10 In peo-
ple with left dominant coronary circulation, the circumflex artery
supplies the inferior surface of the heart and circumflex occlusion
ST segment
depression
DISPLAY 15-2 Causes of Noninfarction
T wave Q Waves 2,3,5–7,10–12,14–16
inversion
Anterior and posterior hemiblock
Horizontal ST Cardiac amyloidosis
segment with Chronic obstructive pulmonary disease
ST-T angulation Hypertrophic cardiomyopathy
Incomplete LBBB
Myocarditis
Tall wide-based
T waves Neuromuscular disorders
Pneumothorax
Pulmonary embolism
U wave Sarcoidosis
inversion
Ventricular hypertrophy
Ventricular preexcitation (Wolff–Parkinson–White
■ Figure 15-25 ECG patterns associated with myocardial syndrome)
ischemia.